This 2019 trial assessed the effects of a low-carbohydrate diet, as implemented in standard clinical practice, on cardiovascular risk in diabetic and prediabetic patients.
The authors include primary care practitioners at Norwood Surgery in the Northern U.K. who began prescribing low-carbohydrate diets to diabetic and prediabetic (and/or glucose intolerant) patients in 2013. Between 2013 and 2018, they tracked the impact of this diet on 154 patients. These patients were given the same guidance as any patients visiting the clinic:
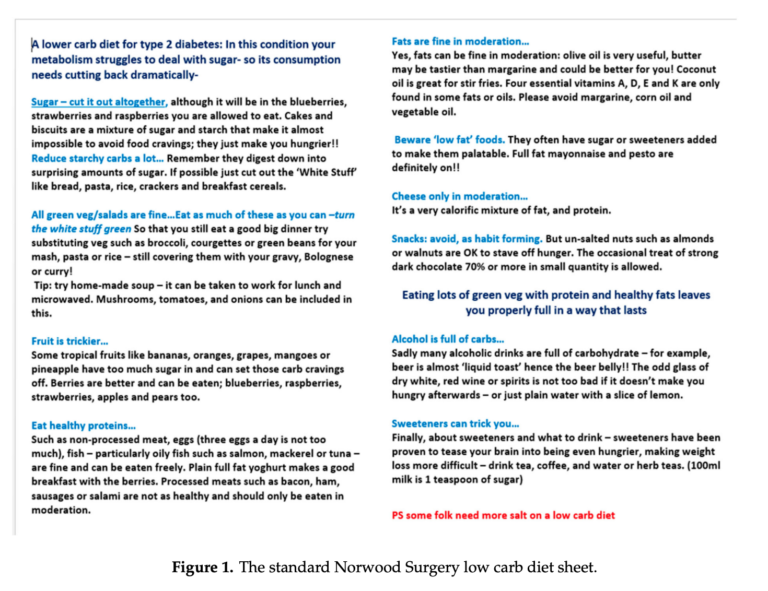
- A low-carb diet sheet providing general guidance on how to follow a low-carb diet
- A follow-up meeting a few weeks later to answer any questions
- Access to monthly 90-minute group sessions
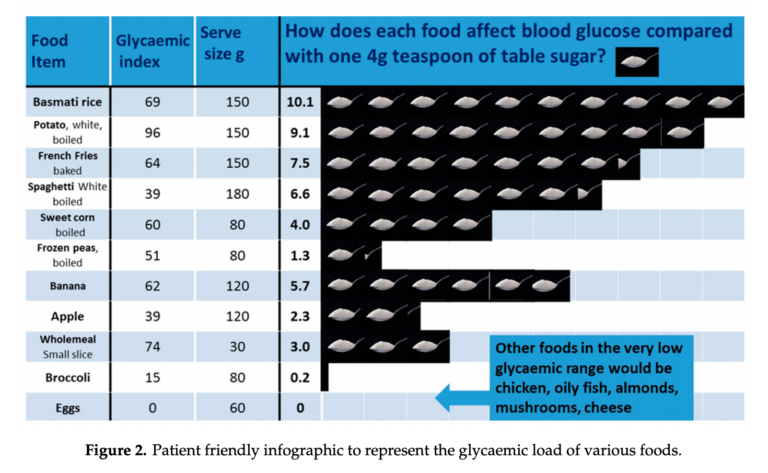
The diet sheet and an attached infographic are shown below. The prescribed low-carb diet emphasized elimination of sugars, dramatic reduction of foods with a high glycemic load, and replacement of these foods with vegetables, some fruit, some dairy, meat, and fats. Compliance was not explicitly measured, though patients reported substantial reductions in carbohydrate intake in periodic dietary surveys.
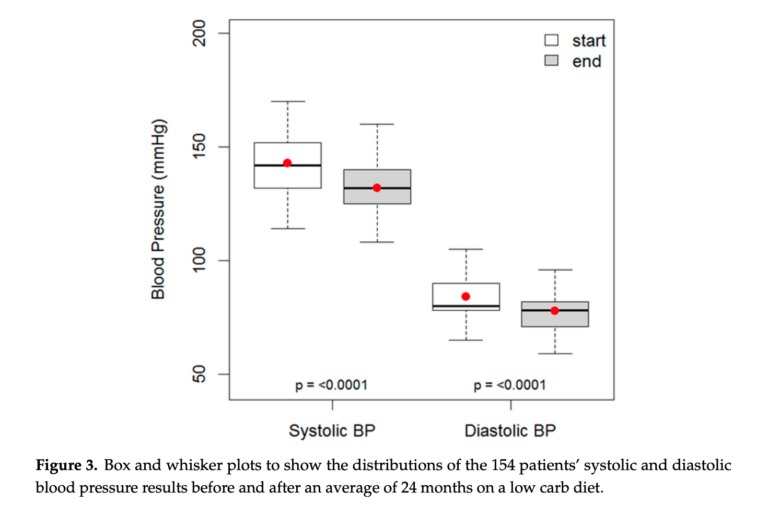
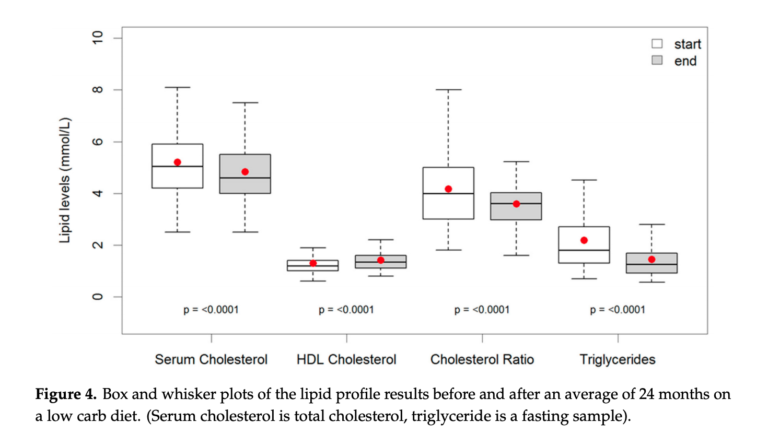
Over a mean follow-up of two years, patients lost an average of 9.5 kg. They also saw reductions in serum cholesterol (0.4 mmol, 7%), triglycerides (0.7 mmol, 32%), systolic blood pressure (10.9 mmHg, 7%), and diastolic blood pressure (6.3 mmHg, 7%). Additionally, they experienced a small increase in HDL cholesterol (0.1 mmol, 7%). All changes were statistically significant.
Notably, the 154 patients were collectively taking 163 drugs for hypertension at baseline; by the end of the trial, 35 of these repeat medications were no longer being prescribed. The authors estimate the actual decreases in systolic and diastolic blood pressure associated with the dietary change alone, correcting for these medication changes, were 14.8 and 8.1 mmHg, respectively. Such blood pressure reductions are associated with a 30% reduction in stroke risk and 20% reduction in future cardiovascular mortality.
This study illustrates the significance of a low-carbohydrate diet in standard clinical practice. This low-carbohydrate diet intervention was extremely simple and low-cost; nonetheless, statistically and clinically significant improvements in a variety of disease risk markers were observed. The total study budget was a mere £7,000 over six years, indicating this sort of real-world trial could be a scalable model for further study of the effects of low-carbohydrate diets. The results alone indicate a low-carbohydrate diet has meaningful cardiovascular benefits in standard clinical practice — future research can uncover other benefits that may be associated with a low-carbohydrate diet or test whether other real-world interventions can improve compliance and thus increase the magnitude of clinical benefits.
Editorial note: The research presented here is consistent with the dietary prescription CrossFit participants and trainers around the world have found to be efficacious in millions of “n=1” experiments (specifically, “eat meat and vegetables, nuts and seeds, some fruit, little starch, and no sugar”). We would not, however, consider this observational study based on self-reported data to be authoritative in and of itself, as it fails to meet the standard of data that is “observable, measurable, and repeatable.”
More authoritative support for similar conclusions regarding the benefits of carbohydrate restriction can be found here: