“‘The method of science is the method of bold conjectures and ingenious and severe attempts to refute them,’ said Karl Popper, the dean of the philosophy of science. Popper also noted that an infinite number of possible wrong conjectures exist for every one that happens to be right. This is why the practice of science requires an exquisite balance between a fierce ambition to discover the truth and a ruthless skepticism toward your own work. This, too, is the ideal, albeit not the reality, of research in medicine and public health.”
—Gary Taubes (1)
In a previous column (2), I showed how Ancel Keys first stole the ideas for the diet-heart and lipid hypotheses from Dr. John Gofman, MD. To conceal his own grave academic limitations — in particular, his lack of training in medicine, cardiology, and lipidology (the study of blood fats) — Keys found the perfect diversion in the discipline of nutritional epidemiology, for which he required no special skills or training. Masquerading behind this covert scientific pretense, he promoted weak associational data from that freshly discovered academic discipline as if it were definitive proof for his — actually Gofman’s — hypotheses. Yet he was fully aware that associational data cannot prove causation except under a few exceptional circumstances, circumstances that Keys’ especially weak associational data could never establish.
Only ever in passing did Keys acknowledge this weakness in his false claims. It was as if he believed that in every other case, associational data could not prove causation, but his claim was different. Since the ideas were his (even if purloined), they had to be correct, even when his proof failed all accepted scientific canons. His truth, he knew, was so absolute, so perfect, it required no human proof. It was biblical. With time, he would collect a bevy of disciples who would faithfully spread his false prophecy to all corners of the Earth.
Keys’ goal was not to use science to discover an ultimate truth for the benefit of humankind. He was rather more mercenary. His fancy was to become the global nutritional megastar “Mr. Cholesterol,” or, as Nina Teicholz describes it, his personal goal was to be “by far, the Greatest Man [in nutrition]” (3, p. 46).
All this was happening in the heady post-war 1950s, when coronary heart disease (CHD) was supposedly reaching “epidemic” proportions in the U.S. and elsewhere. At this time, the premier focus of medical research in the U.S. and the Western world had become the need to find an urgent solution to the CHD crisis.
Keys’ proposed solution was particularly appealing because it was really so very simple. Everyone could easily understand it: Remove saturated fat from the diet. Do this and Keys’ prediction was that the CHD “problem” would disappear: “[If] mankind stopped eating eggs, dairy products, meat and all visible fats … [coronary heart disease would] become very rare” (4, p. 99).
For the record, Keys’ solution at the time (January 1952) was the following:
I would recommend a sharp reduction in all dietary fats without paying any special attention to the cholesterol content of the diet. I would allow the use of an ordinary amount of eggs and milk in cooking, the use of skim milk for cereals and as a beverage, a good daily serving of lean meat or fish, and a boiled or poached whole egg for Sunday; but no butter, cream, oleomargarine, salad oil, mayonnaise, fried foods, gravy, ice cream, chocolate, or pastries made with shortening. Periodic measurements of serum cholesterol may help to judge the severity with which such restrictions should be maintained. (4, p. 99)
Keys confidently provided this advice despite the absence of any evidence at the time to support it. Clearly, he just “knew” what was going to save the world from the scourge of coronary heart disease.
In contrast to Keys’ absolute certainty, one of the world’s leading cardiologists of the day, Dr. Louis Katz, MD, warned that he would prescribe this low-fat, low-cholesterol diet only “when a patient has had two or more attacks of coronary insufficiency and/or myocardial infarction attributable to coronary atherosclerosis, and if that patient has a cholesterol level in the upper limits of normal, or above … . Otherwise, I would not, because I am a firm believer in the view that prohibitions should not be carelessly advocated until such time as it is clearly revealed that the prohibition has a great chance of being beneficial to the patient” (4, p. 99).
Importantly, as a world-leading cardiologist, Katz actually regularly treated patients with heart disease. He also had a penchant for asking difficult (and relevant) questions (5), while Keys had no training in either medicine or cardiology. Yet remarkably, Keys’ unproven opinions would ultimately win the argument over more qualified clinicians such as Katz. This was because Keys had effectively positioned himself as the right man in the right place at exactly the right time.
So when, in the late 1960s, Keys became one of the original beneficiaries of research funding from the newly formed National Heart, Lung, and Blood Institute (NHLBI), he discovered, to his utter dismay (and perhaps horror) that, far from supporting his claims, his brilliantly designed and perfectly executed test — the Minnesota Coronary Experiment (MCE) (6) — comprehensively disproved both his hypotheses. According to Karl Popper’s description that a real scientist is someone imbued with a “ruthless scepticism toward your own work,” had Keys been just such a scientist, this should have been the end of his hypotheses.
The MCE established that the replacement of dietary saturated fat with the polyunsaturated fatty acid (PUFA) linoleic acid, which lowered average blood cholesterol concentrations by 15% to the apparently “safe” level of 175 mg/dL (4.6 mmol/L), had absolutely no effect on heart disease outcomes. Instead, “no differences between the treatment and control groups were observed for cardiovascular events, cardiovascular deaths or total mortality” (6, p. 129).
This finding fatally dispatched Keys’ hypotheses because the MCE established that, when tested in a rigorous and essentially flawless trial, using Keys’ dietary recommendations to lower cholesterol failed to prevent CHD as Keys had promised.
Instead of declaring this inconvenient truth as all honest scientists must, the authors of the MCE report (6) invented two novel explanations that have since become the go-to excuse for nutritional scientists whose experiments disprove their deeply held biases.
First, they declared it is not their theory that is wrong: “Although the study did not show a statistically significant reduction in cardiovascular events or total deaths from the treatment, the authors suspect that it might have shown such a reduction if the period of treatment had been longer in persons in the age range likely to benefit” (6, p. 134, my emphasis).
In other words, in breach of the Popper principle, the authors implied they knew beforehand that their ideas are correct: If the experiment failed to produce the expected results in line with their predictions, then it is not they, the scientists, who could possibly be wrong. Instead, it is clearly the experiment that has failed. And its findings are in error for the very obvious reason that they failed to confirm the authors’ theory.
When they did not find the result they wanted, the MCE authors simply buried the findings as if the study had never been done. The tragedy was that hidden in the data was evidence that the diet was harmful (8). A new analysis by independent scientists established that removing saturated fat from the diet to lower the blood cholesterol concentrations caused measurable harm. The effects were especially marked in those over 65 years of age.
-
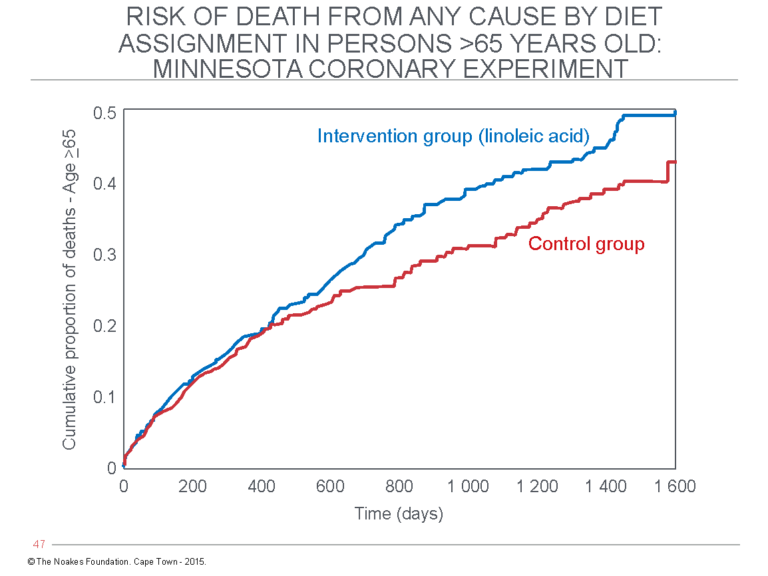
Figure 1: The “recovered” mortality data in the 1968-1973 MCE published in 2016 (52) found no evidence of cardiovascular benefit from the diet that lowered blood cholesterol concentrations. Instead, survival in participants over 65 years old receiving the intervention diet (blue line) was significantly worse compared to the control group participants who continued to eat their usual diet (red line). Reproduced from reference 6.
Had those data been properly analyzed and published in 1976 when they became available, they may have prevented the distribution of the harmful dietary advice that subsequently developed, in particular the 1977 U.S. Dietary Guidelines developed by Senator George McGovern’s hopelessly under-qualified committee (as I discuss subsequently (10)). It is not ethical to prescribe to an individual, let alone to an entire nation, an intervention that is known beforehand to cause harm, even if that harm is only relevant to a minority. This is the foundation of ethical medical practice: First, do no harm.
Like the MCE authors, the directors of the $700-million Women’s Health Initiative Randomized Controlled Dietary Modification Trial (WHIRCDMT), discussed subsequently (11), used post-hoc rationalization when they failed to find any benefit for replacing dietary saturated fat with polyunsaturated fatty acids (PUFAs), even though that dietary intervention also lowered blood cholesterol concentrations (12).
I suspect the WHI authors were certain the WHIRCDMT would provide the ultimate Nobel Prize-winning proof of Keys’ hypotheses (13, p. 60-62). They were confident their deluxe trial, for which no cost had been spared, would finally prove the benefit of a low-fat, cholesterol-lowering diet in the prevention of coronary heart disease (CHD), even though a host of studies pursued over 30 years at a cost of hundreds of millions of dollars of U.S. taxpayer money had stubbornly refused to provide such evidence.
In the end, the WHIRCDMT found that replacing dietary saturated fat causes harm, especially to those with pre-existing heart disease or Type 2 diabetes mellitus (11).
The third study in what should now be referred to as a nutritional holy trinity is the recovered Sydney Diet Heart (recovered SDHS) Study (14). In this study, subjects with a previously documented heart attack were randomized to either a group that continued eating as they always had or to one in which dietary saturated fat was replaced with the polyunsaturated fat (PUFA) linoleic acid, extracted from safflower.
While the original study (15) reported that the diet was neither harmful nor helpful, when the original data were recovered and re-analyzed by independent scientists (14), it became clear the diet had caused harm (16).
These three RCTs — the WHIRCDMT, the recovered MCE, and the recovered SDHS, together costing close to $1 billion — have unequivocally established that removing saturated fat from the diet causes harm. So powerful is the evidence that, in my opinion, it should end the debate.
Any one of these studies should, by itself, have brought an end to the idea that humans should avoid eating saturated fat since saturated fat is the driver of coronary heart disease. Each of the three studies proves that any dietary advice based on Keys’ false hypotheses is not just wrong; it is unethical. Worse, it is not as if we had not been warned.
The first trial of the low-fat diet enriched with polyunsaturated fats was the Diet and Coronary Heart Disease Study Project, popularly referred to as the Anti-Coronary Club Program in New York City. The study (17), reviewed in detail subsequently (18), began in 1957 and continued until 1972.
Unfortunately, in 1961, the trial’s principal investigator, Dr. Norman Jolliffe, died suddenly of a heart attack. While the clinicians who continued the trial after Jolliffe’s death claimed his “prudent diet” reduced the number of coronary events, hidden in their data was one very inconvenient fact: There were more deaths in the group that followed the experimental diet. Clearly, the “prudent diet” had not helped the Anti-Coronary Club members live any longer.
The next published clinical trial of a modified diet to treat patients after heart attack was conducted at a group of Middlesex hospitals in the United Kingdom (19). The tested diet had reduced fat content — there was no substitution of fat with polyunsaturated fats. Subjects in the intervention group were restricted to 40 grams of fat each day, provided by 14 grams of butter, 84 grams of meat, 1 egg, and 56 grams of cottage cheese and skim milk. The diet was not popular: “The diet was often unpleasant … . The main objections were to the skimmed milk, and to the small butter ration … and to the restriction on biscuits and cakes” (19, p. 501).
Patients eating this “unpleasant” diet lost more weight and showed greater reductions in blood cholesterol concentrations, but the incidence of new cardiac events was not different between diet groups. Thus, the authors concluded prophetically: “A low fat diet had no place in the treatment of myocardial infarction (heart attack)” (19, p. 504).
If that conclusion had been accepted in 1965, the world would have been saved 55 years of futile efforts by the National Heart Institute (NHI) and American Heart Association (AHA) to prove the opposite.
The third relevant study was the second to evaluate the replacement of dietary saturated fat with PUFAs in patients who had recently suffered a heart attack (20). This study found that “patients receiving the key treatment (corn oil) fared worse than those in the other two groups: two years from start of treatment, infarction or death had occurred in one-quarter more of the corn-oil than of the control group. This difference closely approaches the conventional significance level (0.1>P>0.05)” (20, p. 1533).
The authors warned: “It is concluded that under the circumstances of this trial, corn oil cannot be recommended in the treatment of ischaemic heart disease” (20, p. 1533).
Thus, already by 1965, three trials of low-fat diets in real heart attack patients living in the real world had found no evidence that the diets benefitted cardiovascular health; instead they found only indications of harm.
Then another eight-year study (21) reported a higher incidence of cancers in a group of men who had replaced saturated fat with vegetable/seed oils. Whereas the number of fatal CHD deaths were higher in the control group for this study, deaths from cancer were increased (31 vs. 17) in the intervention group. As a result, all-cause mortality was the same in both groups, again confirming no benefit and the potential for harm when dietary saturated fat is removed from the diet and replaced by vegetable oils.
The potential link between cancer and diets high in PUFAs (22-40) became a problem for the NHLBI in the 1980s and continues to be studied today (41-43), as does the association between low blood cholesterol concentrations and a range of other medical and behavioral conditions (44-62). Predictably, the cancer-PUFA relationship is never raised by those promoting the AHA/NHI position that the lower the blood cholesterol concentration, the better.
To investigate the matter, or perhaps more accurately, to scotch any speculation that low-fat dietary advice could ever do anything other than good, the NHLBI convened three workshops between 1980 and 1982 (1, p. 54). The NHLBI faithfully concluded “the evidence didn’t imply cause and effect. They believed that high cholesterol caused heart disease and that low cholesterol was only a sign of people who might be cancer-prone because of a genetic predisposition” (1, p. 55). As a result, and very conveniently, they concluded “the data do not preclude, countermand, or contradict the current public health message which recommends that those with elevated cholesterol levels seek to lower them through diets lower in saturated fat and cholesterol” (41; 42, p. 2503S).
In a further NHLBI conference in October 1990, any possibility that adverse outcomes were the direct result of low blood cholesterol concentrations was once more fudged: “Definitive interpretation of the association observed was not possible, although most participants considered it likely that many of the statistical associations of low or lowered total cholesterol level are explainable by confounding in one form or the other. The conference focused on the apparent existence and nature of these associations and on the need to understand the source rather than on any pertinence of the findings for public policy” (43, p. 1046).
In other words, the conference participants reached a consensus based on nothing better than their personal biases that a low blood cholesterol concentration is not a direct cause of any adverse health outcome. Case closed, even in the absence of definitive proof.
Recall, of course, that then as now, the NHLBI had no evidence whatsoever that lowering “elevated” blood cholesterol concentrations with diets low in saturated fat and cholesterol provided any benefits. But any possibility that this dietary intervention might cause harm was simply ignored, as often remains the case today. This is a remarkable achievement for this small group of medical scientists.
As a result, any possibility that interventions that lower blood cholesterol concentrations might also increase risk of death from cancer or other serious medical or abnormal behavioral conditions has been written out of the scientific record.
Burying the Negative Findings From the MCE
Why did Keys and his cronies ignore what should have been very worrying findings from the SDHS and MCE? And why did they fail to uncover and report, as was their scientific duty, the clear evidence of harm in the MCE, as was subsequently detected by C. E. Ramsden et al. (8)? Or the evidence of harm that was clearly apparent in the SDHS, which also was subsequently uncovered by Ramsden and his colleagues (14)?
The son of the first author of the original MCE paper, Dr. Ivan Franz, suggested the following:
My feeling is, when the overall objective of decreasing deaths by decreasing cholesterol wasn’t met, everything else seemed less compelling. I suspect there was a lot of consternation about why (they couldn’t find a benefit). The idea that there might be something adverse about lowering cholesterol (via vegetable oils) was really antithetical to the dogma of the day. (63)
Or in the words of Steven Broste, whose 1981 M.Sc. thesis analyzed the original MCE data:
The results flew in the face of what people believed at the time. Everyone thought cholesterol was the culprit. This theory was so widely held and so firmly believed — and then it wasn’t borne out by the data. The question then became: Was it a bad theory? Or was it bad data? … My perception is that they were hung up trying to understand the results. (64)
A lead author of the recovered MCE, Daisy Zamora, Ph.D., concluded that “had this research been published 40 years ago, it might have changed the trajectory of diet-heart research and recommendations” (64) — a chilling thought.
All this invites the obvious question: If scientists can’t accept the evidence of their own experiments, especially when that evidence runs contrary to their firmly held beliefs, then why do they bother to conduct experiments in the first place? The actions of Keys and his colleagues show they were not disinterested scientists searching for truth. They were pursuing some other purpose.
Had Keys demanded that the data be thoroughly scrutinized and published in the 1970s instead of 46 years later, as was his ethical responsibility, it would have had one significant consequence that, to my knowledge, no modern ethicist has yet identified: It would have forced the termination of all future clinical trials of diets that aimed to lower blood cholesterol concentrations by removing saturated fat from the diet.
Armed with the evidence from the MCE and the SDHS (and later the WHIRCDMT) that removing saturated fat from the diet causes harm, it would have been unethical for any medically trained research scientist to participate in a trial that was known to put the health of even a single trial participant at risk. No future study would have received ethical approval from a University Review Board.
Instead, as a result of Keys’ inaction and his religious certainty that he was correct, many more have been harmed.
As Andrew Mente, Ph.D., posted recently on his Twitter account (@andrewmente): “The basis of science is scepticism; the basis of religion is faith.” Mente was the senior scientist of the Prospective Urban Rural Epidemiology (PURE) study (65), which produced opposite results of those from Keys’ Seven Countries Study (11).
Keys and his acolytes had long since crossed the slender boundary dividing skepticism from faith — that which demarcates science from religion. Already in June 1953, before he had conducted a single test of his hypotheses, Keys confirmed his religious certainty at the Annual Health Conference of New York:
Many factors are probably involved in the clinical appearance of coronary heart disease, but there is no longer any doubt that one central item is the concentration, over time, of cholesterol and related lipids and lipoproteins in the blood. No other etiological factor of comparable importance is as yet identified. (70, p. 1399-1400)
But the references cited by Keys are mainly personal opinions, and none provide definitive support for his contention about cholesterol. In fact, a professor of medicine at the Long Island College of Medicine named William Dock, MD, had a somewhat different opinion: “Today, over most of the earth, want is the rule, and atherosclerosis is being prevented by chill penury. Where a luxus diet prevails, diabetes and atherosclerosis flourish” (71, p. 188). Subsequently he wrote, “By the time thrombosis and clinical disease occur, cholesterol or beta-lipoprotein levels in many populations are relatively less elevated in coronary cases than are the plasma triglyceride levels. The latter affect platelet stickiness, fibrinolysin, and plasma clotting times more than do the beta-lipoproteins” (71, p. 794, my emphasis). So unlike Keys, Dock recognized dietary carbohydrates and fats had different effects on blood cholesterol and triglyceride concentrations, and he cited a study by I. MacDonald and D. M. Braithwaite (72) that showed this.
Gary Taubes neatly describes the trap into which Keys would fall:
Believing that your hypothesis must be correct before all the evidence is gathered encourages you to interpret the evidence selectively. This is human nature. It is also precisely what the scientific method tries to avoid. It does so by requiring that scientists not just test their hypotheses, but try to prove them false. ‘The method of science is the method of bold conjectures and ingenious and severe attempts to refute them,’ said Karl Popper, the dean of the philosophy of science. Popper also noted that an infinite number of possible wrong conjectures exist for every one that happens to be right. This is why the practice of science requires an exquisite balance between a fierce ambition to discover the truth and a ruthless skepticism toward your own work. This, too, is the ideal, albeit not the reality, of research in medicine and public health. (1, p. 24-25)
But for Keys and his acolytes, there was no place for skepticism. Instead, Keys insisted that “each new research adds detail, reduces areas of uncertainty, and, so far, provides further reasons to believe” (1, p. 25).
Albert Einstein, who discovered a universal truth, wrote the exact opposite: “No amount of experimentation can ever prove me right; a single experiment can at any time prove me wrong.”
Keys, on the other hand, believed a single experiment could prove him right, and no amount of contrary findings could ever prove him wrong.
So he always searched for the single study he could market as the definitive proof of his speculative hypotheses. Every other study was irrelevant and, in his mind, could legitimately be suppressed.
So it was that Keys’ religious certainty made him the immaculate disciple for the promotion of what would soon become a politically and commercially driven agenda, the consequences of which have been so catastrophic for global health.
Keys’ Host of Fellow Travelers
The reality is that, on his own, Keys could not have bullied the disciplines of nutrition and medicine into abandoning scientific skepticism for religious certainty. To achieve that fundamental transformation, he needed the active support of many powerful and influential persons and institutions — those who were willing to invest billions of dollars to undertake a specific brand of research designed to promote, not falsify, this new dogma.
For the first 40 years of my professional career, I, probably like almost all medical doctors, was completely blind to the magnitude of this deception and the nature of the forces directing it. Only when I read and re-read the game-changing books by the pathfinders for truth in this matter — Russell L. Smith and Edward R. Pinckney (74), Thomas J. Moore (75), Gary Taubes (1), and Nina Teicholz (3) — did I begin to see the truth, even if at first only dimly.
In the remaining columns in this series, I will highlight the key scientific events over the past 100 years that produced the original fake medical news story: the adoption of Keys’ diet-heart and lipid hypotheses as indisputable medical dogmas.
This happened not just in the absence of definitive evidence but in the face of an irrefutable body of evidence that proves and continues to prove more resolutely every day that both hypotheses are false (74, 76-80).
My aim is to show how this scam unfolded and why a greater public understanding of exactly how we have been lied to for more than 100 years is the sole antidote that can reverse the massive harm to global health these untruths have caused.