Our discovery in 1991 that EAH and EAHE are due to abnormal fluid retention in those who overdrink during prolonged exercise occurred at the most inconvenient moment for the U.S. sports drink industry.
For it happened that at that precise moment, Gatorade had decided to support the American College of Sports Medicine (ACSM) financially. This occurred just four years after the Water as a Tactical Weapon Doctrine, inspired by the U.S. Army Research Institute for Environmental Medicine (USARIEM), had been accepted by the U.S. Army (1). It was also just shortly after the foundation of the Gatorade Sports Science Institute (GSSI) and only five years before the 1996 ACSM Position Stand would advance the Zero-Percent Dehydration Doctrine (2).
The challenge for the industry became the need to sustain the doctrine that drinking ahead of thirst and “as much as tolerable” was healthy in the face of a growing body of evidence disproving this dogma (3).
One solution would be to spin the theory that the main cause of EAH and EAHE is large sodium losses, especially in those whose sweat contains abnormally high concentrations of salt— the so-designated “salty sweaters.” This would be based on a novel hypothesis (4) originally developed by Drs. Doug Hiller and Bob Laird, who at the time were the senior physicians in charge of medical care at the Gatorade-sponsored Hawaiian Ironman Triathlon.
Remarkably, despite all the conflicting evidence, this erroneous theory continued to be promoted by the GSSI as recently as 2008, when I last checked (5).
In 1998, Laird was kind enough to invite me to be present at that year’s Hawaiian Ironman Triathlon, after which he sent me home with a copy of all their carefully collected data on athletes requiring medical care in the 1983-1998 races.
While going through the data, I was reminded that some time after our first publication on EAH and EAHE in 1985 (6), I was invited by a medical journal editor to review a scientific paper on cases of EAH and EAHE occurring at the Hawaiian Ironman Triathlon.
In my review I pointed out that the anonymous authors did not understand their data. For while they were claiming that EAH was caused by “dehydration,” their data clearly showed the opposite: EAH developed in triathletes who either did not lose any weight or who gained weight during the race. The authors chose to ignore my exposé of their inconvenient finding. As a result, their error was never corrected and their paper was never published, simply because it was quite wrong.
Was their cognitive dissonance occasioned by a dependence on funding from Gatorade to sustain the Hawaiian Ironman Triathlon in those early years of its existence?
In 1998, thanks to Laird, I had a chance to analyze the complete record of cases of EAH and EAHE at that race.
Our analysis showed that the Hawaiian Ironman Triathlon was the single greatest contributor to the EAH and EAHE epidemic after 1981 (7)—which was predictable because the drinking guidelines for that race reflected the ACSM Position Stands’ advice to “drink as much as tolerable” and promoted fluid intakes as high as 2 L/hr in larger athletes.
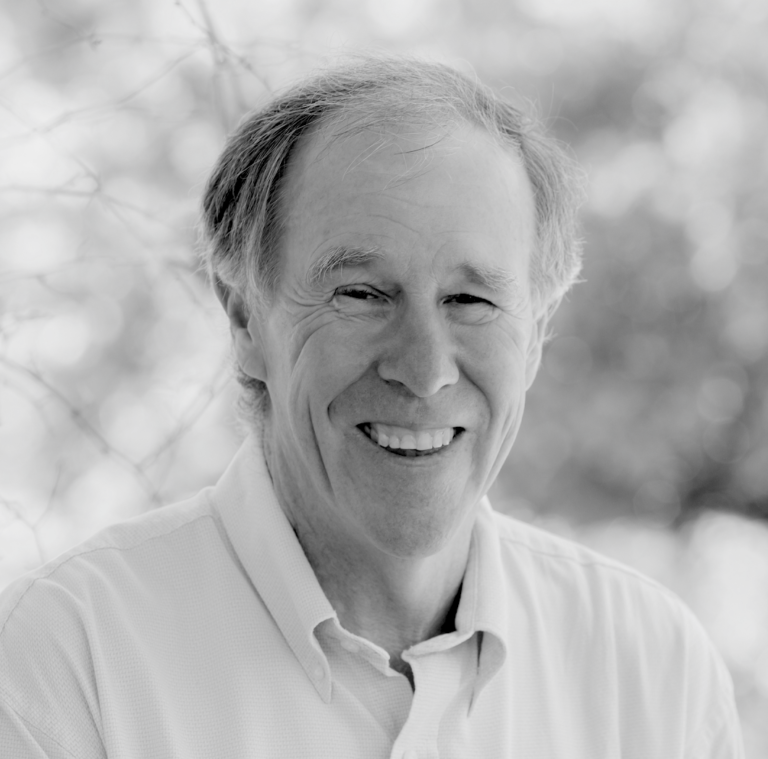
The data showed that between 1983 and 1998, there had been more than 17,000 finishers in the race (Figure 1, left panel), and of these, close to 5,000 (~30%) had been treated in the medical tent at the race finish (Figure 1, right panel). Astonishingly, nearly 2,400 finishers had their blood sodium concentrations measured, a great tribute to Laird and his team.
Of those whose blood sodium concentrations had been measured, approximately 800 were below 135 mmol/L, indicating the presence of EAH. Of these, about 500 were below 135 mmol/L but above 128 mmol/L, indicating increasingly severe EAH. Remarkably, about 300 finished these races with blood sodium concentrations below 128 mmol/L, indicating highly probable EAHE. The two smallest categories, each with fewer than 100 triathletes, comprised athletes with elevated blood sodium concentrations of >145 mmol/L, indicating dehydration, and those athletes who were hospitalized.
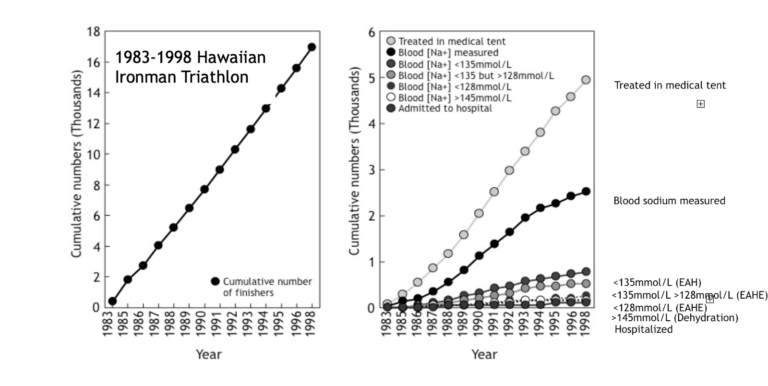
Figure 1, left panel: Cumulative number of finishers in the Hawaiian Ironman Triathlon. Right panel: Cumulative number of athletes (i) treated in the medical tent; (ii) with blood sodium measurements; (iii) blood sodium concentration less than 135 mmol/L (EAH); (iv) blood sodium concentration less than 135 mmol/L but greater than 128 mmol/L (borderline EAHE); (v) blood sodium concentration less than 128 mmol/L (EAHE); (vi) blood sodium concentration greater than 145 mmol/L (dehydration); (vii) hospitalized.
At both the 1989 and 2005 races, there were data for body-weight changes and changes in blood sodium concentrations (Figure 2). Both showed the well-established phenomenon that blood sodium concentrations fell the most in athletes who gained weight during the race and rose the most in those who lost weight and were therefore dehydrated.
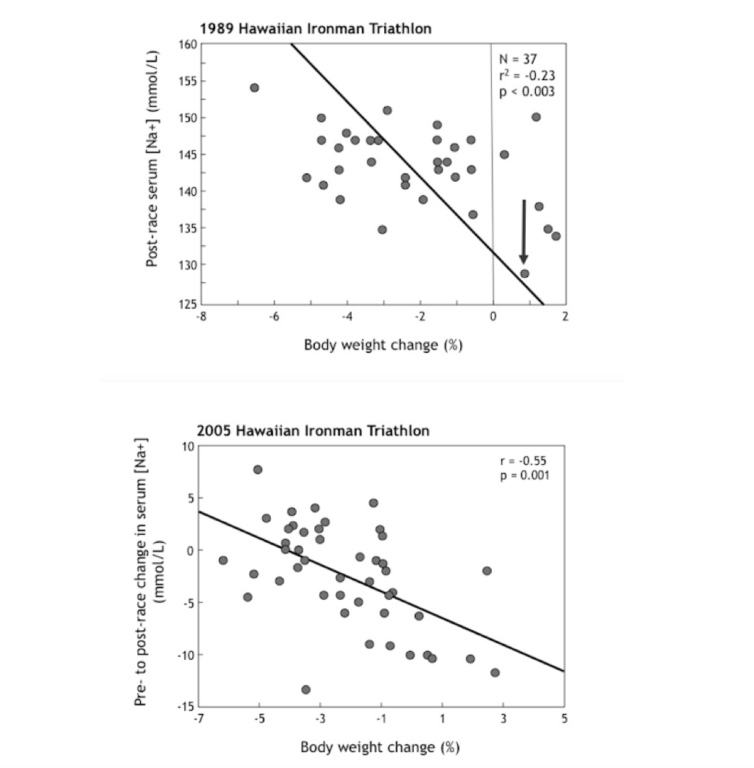
Figure 2: In both the 1989 (top panel) and 2005 (bottom panel) Hawaiian Ironman Triathlons, there was an inverse relationship between weight changes during the race and the post-race serum sodium concentrations, confirming that changes in body water content are the key regulators of blood sodium concentrations during prolonged exercise (Reproduced from reference 7, p. 261, Figure 9.8).
In the face of this evidence, there was a commercial need to come up with a novel explanation for why athletes need to continue drinking copious amounts of (sponsors’) sodium-containing sports drinks during exercise. The condition of salty sweating in those with cystic fibrosis (CF) offered the perfect faux explanation.
Disproof of the Faux “Salty Sweater” Explanation for EAH and EAHE
Professor Dorothy Andersen was the first to discover that CF—a progressively fatal human condition in which certain bodily secretions, especially those in the lungs and intestines, are excessively thick and tenacious—is a genetic disorder (8). During an unusually hot summer in New York in 1949, Andersen noted that a number of her young children with CF were stricken with “heat prostration” (9). Symptoms of the condition included unexplained fever with “severe dehydration and vasomotor collapse” (10, p. 549). On the assumption that this distress was caused by severe (volume depletion) dehydration caused by pure salt losses, a junior professor working with Andersen, Paul di Sant‘Agnese, then established that the sweat glands were the source of their abnormally large sodium losses (10-13).
These early studies therefore established that persons with CF are intolerant of heat since they lose excessive amounts of sodium in sweat and so are unable to regulate their sweat sodium losses, although they can reduce urinary sodium losses in the same way healthy humans do. This inability to conserve sodium impairs their capacity to acclimatize to heat since heat acclimatization does not occur without sodium conservation (14,15). Even so, a number of patients with CF have overcome this disadvantage and even completed 26-mile marathon footraces; the feats have stimulated studies of the exercise response in persons with CF.
These studies have established that CF patients have normal thermoregulatory, cardiovascular, renal, and hormonal responses to exercise and heat stress but lose more sodium chloride in sweat than is normal since their sweat sodium concentrations were higher (>70 mmol/L) than controls (<50 mmol/L) (16). Yet their kidneys decrease their sodium excretion normally during exercise (since the mechanisms of sodium conservation are different in the kidneys and the sweat glands, and the kidneys are unaffected by CF).
In addition—and critically importantly—with one exception (16), studies have shown that persons with CF are able to maintain their blood sodium concentrations within the normal range during exercise (17-21), even when they were forced to drink “to stay ahead of thirst” during exercise (19). This led, in one case, to a CF runner gaining 2 kg of weight during the seven hours it took him to complete a 26-mile marathon (18).
In one study, a small fall in the blood sodium concentration was not affected by the ingestion of a sodium-containing drink of up to 50 mmol/L, although CF patients drank more of the highly concentrated solution and so became less “dehydrated” (20).
Although the authors tried to spin their finding as evidence that CF patients are at risk of developing EAH if they do not drink a concentrated sodium-containing drink during exercise, their data did not support this conclusion.
Rather, that study found that children with CF were able to regulate their blood sodium concentrations perfectly adequately during 80 minutes of exercise in severe heat without any significant change, even when they drank only water. Perhaps the reasons why the authors thought CF patients need to drink a sports drink during exercise to prevent EAH was because the senior author of this series of papers, the late Dr. Oded Bar-Or, enjoyed a long and cozy relationship with Gatorade and the GSSI.
So these studies fail to support the hypothesis that “salty-sweating” CF patients are unable to regulate their blood sodium concentrations and develop “dehydration hyponatremia.” Rather, they established that CF patients are able to regulate their blood sodium concentrations during exercise regardless of whether they ingest solutions with high sodium content, which further confirms that the blood sodium concentration is not affected by the level of the sodium deficit that develops during exercise.
If EAH does not occur in CF patients during exercise, then, unfortunately, the Hiller-Laird hypothesis that “salty sweating” and “dehydration” cause EAH has to be wrong.
This, however, did not deter another Gatorade and GSSI stalwart, Randy Eichner, MD, from subsequently developing his own unique theory (22) that “salty sweating,” on a genetic basis, probably exists in a large percentage of the population, placing them at high risk of developing “dehydration EAH” during exercise.
Dr. Randy Eichner’s Proposition Regarding Dehydration-Induced EAH and EAHE
Figure 3 explains how the sweat glands convert a filtrate of blood into a hypotonic sweat solution.
Figure 3 – Sweat gland function: The most widely accepted model of sweat gland function suggests that fluid from the interstitial space is secreted into the secretory coil of the sweat gland (left side of figure). This fluid has the same sodium chloride concentration as the interstitial fluid/blood. This secretion is stimulated primarily by the action of cholinergic fibers of the sympathetic nervous system; adrenergic fibers of the sympathetic nervous system play a lesser role in sweat secretion. Once the sweat secretion enters the reabsorptive duct, water and especially sodium is reabsorbed so that the final secretion is hypotonic. The extent of sodium reabsorption is regulated by the hormone that Dr. Jerome Conn discovered, aldosterone. Patients with CF have two defective genes for the cystic fibrosis conductance regulator (CFTR) and are therefore unable to secrete a hypotonic sweat. Carriers of one defective CFTR gene secrete sweat with a normal sodium chloride concentration, disproving the hypothesis that persons with one defective CFTR gene are “salty sweaters” on a genetic basis (Redrawn from reference 23) .
Eichner proposed the theory that “athletes with ‘salty sweat’ are prone to sodium deficits, heat cramping, plasma volume contraction, and notably in endurance events, hypovolemic hyponatremia, sometimes called ‘hyponatremic dehydration’” (22, p. S36). He further proposed that in certain populations, in particular among those who originate from northern European countries, a single defective CFTR gene is present in about one person in 20. As a result, he argued, “up to one white person in 20” has one defective CFTR gene, and this means that “in a marathon with 20,000 white runners, up to 1000 runners may be genetically programmed for ‘salty sweating.’ These runners may risk hyponatremic dehydration during the event” (p. S37).
To sustain this erroneous argument, Eichner needed evidence that those who are heterozygous for this defective CFTR gene, that is those who have one defective and one good CFTR gene, secrete a “salty sweat.” Thus, he wrote, “Limited studies suggest that heterozygotes lose elevated amounts of salt in sweat” (24).
In fact, there is not a limited number of studies, and the best of these studies show that there is no difference in sweat sodium concentrations for those who either have one or no defective CFTR gene (23-29). As Paul Quinton writes, “We learned that sweat salt concentrations cannot be used to predict the heterozygote status of an individual and that obligate heterozygotes seem almost, if not, normal” (23, p. 215). This is shown in Figure 4.
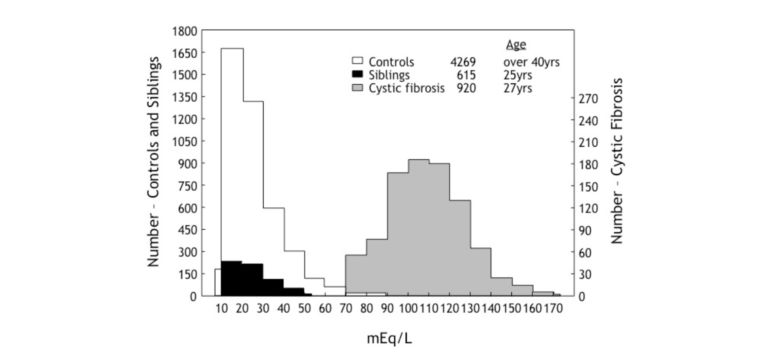
Figure 4: This diagram compares the sweat sodium concentrations in persons with CF, in healthy controls, and in healthy siblings of patients with CF. Since they are healthy, these siblings will have inherited only one defective CFTR gene from their parents. Contrary to Eichner’s theory, persons with one defective CFTR gene have sweat sodium concentrations that fall within the normal (control) range (Redrawn from reference 25).
There is no genetic basis for “salty sweating.” Instead, if an athlete presents with a high sweat sodium concentration, it must be because he or she is eating a high-salt diet (as shown by Conn’s studies (30)) and is in a positive sodium balance so that an increased loss of sodium in sweat is used to balance that excess.
“Salty sweating” is a sure sign of a sodium excess in the body, not of a potential to develop a sodium deficit as Eichner, on behalf of Gatorade and the GSSI, would like us to believe.
Gatorade and the GSSI’s Marketing Campaign
The proof that salty sweating is not a disease but merely a normal biological response to a high salt intake did not deter Gatorade and the GSSI from creating a marketing campaign aimed at convincing the public otherwise.
So in 2008, the GSSI set out to “prove” that a range of superstar athletes, either funded directly by PepsiCo/Gatorade or involved in sports funded by PepsiCo/Gatorade, were all likely to develop sodium deficiency during their chosen activities.
They developed a marketing campaign to show that Tiger Woods, Maria Sharapova, Ronaldinho, Ricky Ponting, Loris Capirossi, Jean-Sébastien Giguère, Yao Ming, Mia Hamm, Peyton Manning, Derek Jeter, and the Chelsea Football team are all at risk of becoming salt deficient during golf, tennis, soccer, etc., and so all need to ingest salt during their different forms of exercise (31, 32).
The studies I have presented in this series establish that (i) sodium balance cannot be determined by measuring only sweat losses since urine is the major source of daily sodium losses in all humans, including athletes eating diets that contain sufficient salt; (ii) it is the absence of salt in urine and sweat, not its overabundance (“salty sweating”), that indicates the presence of a sodium deficit; and (iii) sodium deficiency will not occur in free-living humans, regardless of how much they sweat.
By measuring only sweat sodium losses, the GSSI “experts” who studied these elite athletes already knew what the outcome of their studies would be. And with a heavy dose of spin, they were able to convince Tiger Woods and a few other sporting luminaries, and through them the world, that salt deficiency and “salty sweating” are real phenomena, not the product of the advertising agencies on Madison Avenue.
Thus, in January 2009, Gatorade announced that it had developed a “new collaboration to develop Tiger-inspired sports performance beverages for athletes at all levels, beginning with the launch of new Gatorade Tiger, a Gatorade Thirst Quencher sub-line that will be launched in March 2008” (33, p.1). The company claimed that the new Tiger sub-line would “provide advanced hydration (fluids and electrolytes) and carbohydrate energy to fuel athletic performance” (p.2).
As the first step in cementing this relationship, Woods underwent sweat analysis testing with the GSSI. This, the GSSI claimed, showcased “his dedication to this collaboration and to improving any aspect of his training and competition. The in-depth (but without urine sampling, my addition) scientific testing, conducted by scientists from GSSI, was designed to shape Woods’ own specialized hydration and nutrition strategy. A measurement of sweat rate, sweat electrolyte concentration, fluid and electrolyte balance and energy needs were analyzed during a vigorous round of testing” (p.2).
Dr. Bob Murray, Ph.D., then explained the noble goals of this unique collaboration:
As we have done with many athletes, our testing with Tiger will help him prepare for, and recover from, his toughest workouts and most intense competitions — by meeting his hydration, recovery and energy needs. Not only will Tiger personally benefit from our sports performance testing, but we continue to build our overall knowledge about athletes at all levels and all sports. Of course, this research with Tiger will also help shape the developments of the products under his signature line. (p.2)
Clearly Tiger must be a “salty sweater” since the improvement that Gatorade Tiger brought to the Gatorade range was a 25% increase in electrolyte concentration in order “to deliver advanced hydration that helps people stay on top of their game, both physically and mentally,” a spokesperson for Gatorade named Paul Dalessio enthused (p.1).
Sadly, events of November 2009 led ultimately to the termination of this relationship in March 2010 and robbed the sporting world, golfers especially, of a novel sports drink designed specifically to improve their golf by allowing them to drive further, hit straighter, chip more accurately, and hole every putt.
Maria Sharapova was the next elite athlete in need of an individualized, advanced hydration plan. During an on-court testing session, GSSI scientists conducted two tests on Sharapova: a sweat analysis test and a hydration assessment test. She apparently appreciated the efforts of the GSSI scientists: “As a professional athlete you always want to find those little percentages that can make you perform better. GSSI does an amazing job of making sure that athletes stay hydrated. They helped me understand that I need to replace more than just water” (34, p.1).
But when pressed, a GSSI scientist was unable to explain what unique information was gleaned from this testing (p.2).
Other athletes to visit the GSSI better to understand their individual hydration needs were Los Angeles Galaxy and “U.S. Men’s National team superstar” Landon Donovan (35). As a result of the testing, Donovan discovered that he sweated “an average amount.” However, he explained,
I have an above-average sweat sodium concentration, which means I am a ‘salty sweater.’ I also learned that while I do drink enough before a workout, I don’t drink enough during and afterwards to hydrate myself. So, making subtle changes, like eating a saltier diet during heavy training, replacing more of my sweat losses, and making sure to hydrate fully after activity and before my next match can really help my performance. (35, p.2)
But the effects of an increased salt intake on Donovan’s performance were not actually measured—only his sweat sodium concentrations were.
Motorcycle racer Loris Capirossi of the Gatorade-funded Ducati Corse team underwent studies during training and competition in Italy. GSSI scientist Nicola Sponsiello opined:
Ducati’s sweat test is a very important opportunity for GSSI since it is the first time that we can get a precise survey of the needs of this sport … . Motorbike pilots are a category of athletes that is particularly subject to dehydration due to special sportswear. Understanding how many liquids and minerals they lose is important to supply the Ducati pilots and staff suggestions to improve performance and prevent loss of attention. (36, pp.1-2).
Jean Sebastian Giguere, goalkeeper for the Anaheim Ducks NHL team, visited the GSSI to understand why he developed dizziness, cramping, and fatigue during games. As a result of these tests, “Giguere learned that although he was drinking water he was not replacing the electrolytes lost in his sweat. To stay hydrated and replenish his electrolytes, the GSSI scientists recommended he drink a properly formulated sport drink, like Gatorade, before, during and after a game or workout” (32, p.1). Giguere contributed the following:
Dehydration is quite an issue in hockey but not enough players pay attention to it. Once you become dehydrated it’s impossible to compete with those players who are fully hydrated. When I get dehydrated it really doesn’t feel great! My ears get plugged and I start getting dizzy. The headaches follow and I know cramps aren’t too far behind. A lot of time I feel like I’m going to vomit either on the ice or in between periods. No matter what sport you’re in, I think hydration is the number one priority you should focus on, along with healthy eating. It gives you energy and helps you recover quickly for the next game. (34, p.2)
Giguere does not address the apparent paradox of vomiting when dehydrated. Vomiting causes, it is not caused by, dehydration.
Australian cricket fast bowler Brett Lee also underwent testing at the GSSI, since, “For Brett, hydration is crucial. He has to perform all day in some of the world’s hottest climates, so he was eager to discover his body’s needs and how to maximize his performance” (37, p.1).
The testing, not unexpectedly, showed that Lee is a “salty sweater” as he lost about 1.3 g of sodium per liter of sweat (59 mmol/L). This “salty sweating” was also diagnosed as the cause of his muscle cramping.
As a result of this testing, Lee claimed to have learned the following:
I used to drink plain water. Water’s great but with water you get to a certain point when your body feels like it’s hydrated. It switches off the thirsty feeling so you don’t drink any more but the truth is you haven’t hydrated properly and you can pay for that later. Since I’ve been drinking to a plan the body feels a lot better, I’m better hydrated and I’ve been using Gatorlytes which is extra sodium and that’s exactly what’s been taken out of me. You do lose a lot of sweat and a lot of salt so it’s a matter of putting that sodium back in and since I’ve been doing that over the last couple of years I think I’ve had only one cramp.
This raises the question of why, if he was cured already “a couple of years ago,” he needed to submit himself to this testing.
The sadness of all this is that the science proves all these statements wrong. Each of these statements represents aggressive marketing with compromises of the scientists and athletes whose carefully scripted statements are driven, not by science, but by commercial interests.
If there is too much salt in sweat, it is because there is plenty of salt in the diet. Hence, all these elite athletes received the incorrect information.
Presumably they were well rewarded for ingesting more salt than they need—and also for misleading the public that trusts their opinions.