As I detailed in the previous column (2), the textbook on heart disease by the world’s premier cardiologist, Dr. Paul Dudley White (3), shows that by 1946, neither he nor anyone else had yet come up with a theory about how and which dietary factors might influence the development of coronary atherosclerosis.
Yet, when he was called to President Dwight D. Eisenhower’s bedside on Sept. 25, 1955, White was aware the low-fat, low-cholesterol, high-carbohydrate diet he was prescribing was experimental. So what happened in such a short time to convince White this experimental diet was sufficiently safe and effective that one of the most powerful politicians in the world could be an ideal guinea pig on which to test it?
Enter Ancel Keys
The answer is that it was into this nutritional knowledge vacuum in the early 1950s that one dominating figure, Ancel Keys from the Laboratory of Physiological Hygiene at the University of Minnesota in Minneapolis/St. Paul, would insert himself. The result was that not only would President Eisenhower be prescribed the untested but “scientific” diet Keys had dreamed up, but for the next 70 years and perhaps beyond, Keys’ influence would be the greatest single factor determining what humans would, in future, consider a healthy diet.
Keys had no medical training, and his previous major academic contribution was a monumental, indeed classic, study of human starvation in conscientious objectors in the U.S. in World War II (4). I suspect — perhaps unfairly, perhaps not — that Keys became interested in researching human heart disease for a very pragmatic reason.
On June 16, 1948, President Harry Truman signed the National Heart Act into law. The act created the National Advisory Heart Council and the National Heart Institute (NHI). Six weeks later, the NHI became one of the six newly created National Institutes of Health (NIH), tasked with “responsibility for the administration of all research and training activities related to heart disease” (5, p. 219). The formation of the NHI produced a sudden influx of money chasing what was then a small cadre of heart disease researchers. As T. M. Olszewski explains, “When President Truman signed the National Heart Act into law, he effectively endorsed this perception of a public health crisis and opened the funding floodgates for researchers studying the diagnosis, treatment and prevention of heart disease” (p. 220). Most of this money would initially be granted to researchers studying coronary atherosclerosis and coronary heart disease.
Keys probably saw his opportunity; he certainly did not waste any time. In fact, he was even a little ahead of the game. His first study of potential factors linked to heart disease, the Minnesota Business and Professional Men Study (6), was launched in 1947 with major government funding, as was his earlier starvation study (4).
Initially, Keys had discounted any potential role of diet in the development of coronary artery disease. The evidence is available in his statement from October 1949 that a very low-fat, low-cholesterol diet “reduces the blood cholesterol in a few weeks, but the diet would scarcely support life indefinitely, even if it could be tolerated — no meat, fish, eggs, milk, cheese, or anything made from these materials.”
“We conclude,” he explained, “that the control of cholesterol in the body must be generally sought in the body itself and not through dietary measures. The dietary damage from eliminating meats, eggs and dairy products may be a real hazard. The possibility of useful effect on arteriosclerosis of such a diet seemed to be remote indeed” (7, my emphasis). He continued: “There you are. If you are a vegetarian to hold down cholesterol you are vegetating in a field of delusion.”
But over the next few years, Keys’ thinking would radically alter, perhaps for the last time.
So within just three years, Keys converted from what would now be termed a “cholesterol denialist” to the world’s most vigorous proponent of the opposite: the concept that too much cholesterol and fat in the diet is the key driver of heart disease (the diet-heart hypothesis) through its (supposed) action in regulating blood cholesterol concentration. According to Keys’ hypothesis first proposed in his now classic 1953 paper (8), elevated blood cholesterol concentration caused by a high-fat diet “clogs” the coronary arteries, causing coronary heart disease (CHD) (the lipid hypothesis).
From a distance of 66 years, and without the opportunity to personally interrogate Keys, I suggest there were two factors that drove Keys to make this radical change in his thinking.
There is zero evidence that, at any time during the rest of his life, Keys was prepared to change his mind in response to novel information about diet and health. In fact, quite the opposite. He was obdurate to any evidence that disagreed with his biases, and hostile and dismissive of anyone who challenged his hypotheses. As Gary Taubes has argued, “Keys, Stamler and their supporters based their belief on the compelling nature of the hypothesis supplemented only by the evidence in support of it. Any research that did not support their hypothesis was said to be misinterpreted, irrelevant, or based on untrustworthy data” (9, p. 25).
So what were the two key factors that caused Keys to change his mind so radically between 1949 and 1953?
The first was the passage of the National Heart Act, which suddenly released a flood of money to support U.S. researchers interested in CHD. Keys had completed his epic wartime research on human starvation (4) and was in need of a new direction. What better option than to follow the money into heart disease research?
The second was that others were busy formulating the original ideas, the diet-heart and lipid hypotheses for which Keys would ultimately attract global notoriety. To be remembered for posterity, Keys would need to usurp these ideas and, just perhaps, write their originators out of history — especially since most of his competitors were rather more qualified than he to be undertaking this research.
Clearly, his reading (10) of a series of papers (11-16) from different authors, some of whom linked the reduction in rates of CHD with dietary deprivations caused by World War II, clearly stimulated his interest in the possibility that dietary animal fats and cholesterol might be linked to rising rates of CHD in the U.S. and elsewhere. But when he read the entirely novel research coming out of Dr. John Gofman’s laboratory at the University of California in Berkeley since August 1950 (17-22), he knew he had a titanic battle on his hands.
Gofman was far better qualified to research dietary factors contributing to CHD. After all, by August 1950 (17), Gofman had discovered and described the lipoproteins, the molecules that transport cholesterol and triglycerides in the bloodstream. He had also shown that a particular lipoprotein fraction was overrepresented in persons with heart disease and that this fraction could be reduced by a low-fat, low-cholesterol diet. Moreover, Gofman had an entire research laboratory and a dedicated stream of funding to advance this research direction rapidly. If anyone was a front-runner to receive the funding support of the NHI and be the chosen leader in this field, Gofman had to be that candidate.
Keys would have known he had to act very quickly if he wanted to be one day remembered as the Nobel laureate who saved the world from the growing epidemic of CHD. Time was short; he had none to waste.
Dr. Haqvin Malmros of Sweden proposes A rudimentary diet-heart hypothesis
The following paragraph, first presented in March 1954, is the key evidence in Keys’ early writings showing from where he first “borrowed” the diet-heart and lipid hypotheses:
In view of the obvious importance of the serum cholesterol concentration, it is interesting that this is reduced in populations on short rations and that famine victims almost invariably have very low serum cholesterol concentrations. The fact that atherosclerotic heart disease diminished sharply in many countries on restricted rations during World War II (11-13) is undoubtedly of major significance … whenever a population is faced with a restricted food supply, the character of the diet tends to change even more than its total caloric content. The greatest and most invariable dietary change in famine, and under such conditions as those of World War II (WWII) in much of Europe, is the replacement of fats by carbohydrates (4, 12). (10, my emphasis)
His reference to Haqvin Malmros’ 1950 article (11) is of the greatest historical importance. There, Malmros describes the intellectual foundation of what would become known for generations after as Keys’ diet-heart hypothesis. Malmros wrote:
The consumption of milk and dairy products as well as other foodstuffs rich in cholesterol is very different even under peace conditions in various parts of the world. There should accordingly be less arteriosclerosis among the races that live mainly on a vegetable diet … . Following abundant supply of high cholesterol food there would seem reason to expect an early appearance of atherosclerosis … . If the cholesterol content of food has any significance for the origin and course of arteriosclerotic vascular diseases, the critical years associated with the war ought to be reflected in the mortality curves of certain countries while they should have no effect upon the curves for the countries in which the supply of foodstuffs has been normal. (139-140)
Malmros began by describing how Dr. F. Henschen (14) associated the decline in CHD death rates in Stockholm during WWII with “the rationing of foodstuffs, which during the years 1942-1943 led to a reduction in the consumption of butter, eggs and meat” (11, p. 140-141).
Malmros then presented a graph (Figure 1) showing “death rate from arteriosclerosis” fell in Sweden, Finland, and Norway during the WWII but continued to increase in the U.S. during the same period while remaining relatively unchanged in Denmark.
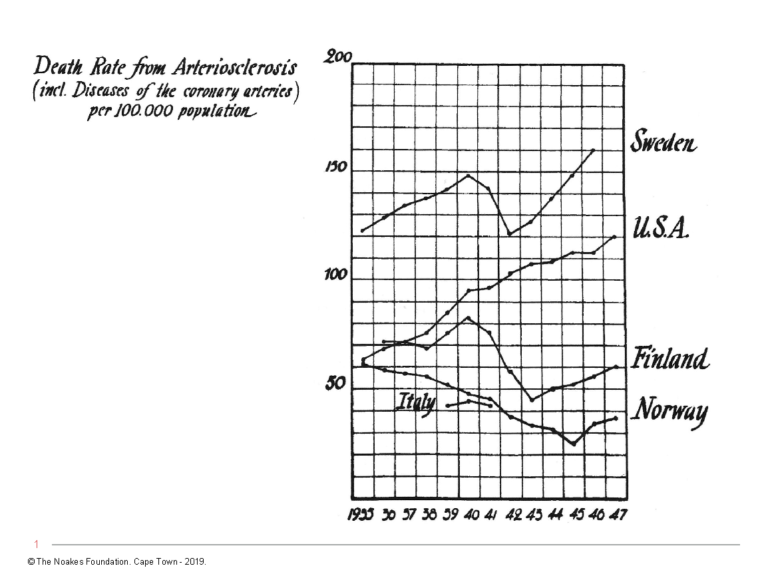
Figure 1: Death rates from arteriosclerosis fell progressively during the years of WWII (1939-1945) in Sweden, Finland, and Norway but showed no such fall in the U.S. Death rates also did not fall in Denmark (data not shown). Reproduced from reference 11.
Next, Malmros showed that whereas the consumption of eggs and dairy (excluding butter) rose in the U.S. while total fat consumption stayed relatively constant (Figure 2, left panel), the opposite occurred in Sweden, Norway, and Finland (Figure 2, right panel). Denmark presented a mixed picture.
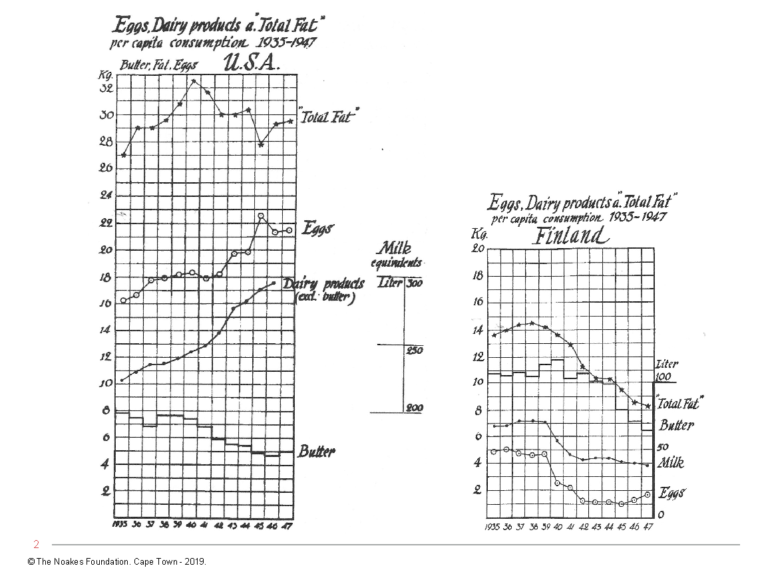
Figure 2: The annual per capita consumption of total fat, eggs, and dairy products, excluding butter, rose or was unchanged during WWII in the U.S. (left panel) but fell steeply in Finland (right panel) during the same period. Changes in the consumption of these foodstuffs in Sweden and Norway, but not in Denmark, followed the same pattern as in Finland. Reproduced from reference 11.
From Figures 1 and 2, Malmros naturally wanted us to draw the conclusion that reduced consumption of eggs and butter explained why heart disease rates fell in Sweden, Norway, and Finland but not in Denmark and the U.S. during WWII.
Malmros made another important point that continues to be glossed over or ignored. He wrote:
It is remarkable that no latency period of appreciable length is found between changes in the composition of the diet and displacements in the course of the mortality curves … . Formerly arteriosclerosis was regarded as a phenomenon that slowly developed with age … possibly it also begins acutely … . It is conceivable that such acutely appearing plaques may grow in a comparatively short time and perhaps after merely a few months produce serious local disturbances of the circulation in, for instance, the coronary vessels. (150-152)
[In fact, it is now understood the development of an acute heart attack requires that an atherosclerotic plaque in any one of the three coronary arteries must rupture, inducing a thrombus (clot) in the affected coronary artery (coronary thrombosis). The point is that plaque rupture is a different biological phenomenon than the development of underlying coronary atherosclerotic plaque. It is entirely possible that conditions produced by an altered diet and other deprivations of war might protect against plaque rupture without altering the underlying coronary atherosclerosis. This point is assiduously ignored in most analyses of how different interventions, including diet, might reduce the risk of heart attack without necessarily altering coronary atherosclerosis.
Interestingly, rates of heart disease in the U.S. began to fall sharply in the 1960s following four decades of a progressive increase. The fall matched the reduction in cigarette consumption and, after 1968, the reduction in consumption of dietary trans fats. But the reduction in heart disease rates occurred too soon after these two interventions to suggest it was caused by an immediate reversal of existing coronary atherosclerosis. It is more likely that the avoidance of smoking and trans fats reduced heart attack rates by acting on the processes of plaque rupture and coronary thrombosis.]
Malmros concluded: “We ought to avoid all luxury consumption of high-cholesterol food stuffs. Especially the combination of eggs and cream, butter and other fats would seem to be risky … . There is much which goes to show that in Denmark, Sweden and the U.S.A the consumption of eggs, butter, milk and other animalic fats is at present too high and may involve serious risks for public health” (p. 153). This sounds rather like the message Ancel Keys would start to preach three years later (8).
In describing the reduction in deaths from heart disease in Norway, in January 1951 A. Strom and A. R. Jensen added more evidence to support Malmros’ evolving diet-heart hypothesis:
[Strom 1948] (15) shows that during the war there was a considerable decline in the consumption of meat and meat products, whole milk, cream, margarine and other fats (but not butter), cheese, eggs, fruit and berries, sugar, and coffee. On the other hand, there was a rise in the consumption of fish, skimmed milk, cereals, potatoes, and vegetables. The average calorie content of the food eaten fell from 3470 per man value per day in 1936-37 to 2850 in 1942-45. This led to widespread loss of weight. The calorie reduction was chiefly in the fat component, which fell from 159 to 71g. per day; and the cholesterol content was reduced accordingly. The average protein content of the diet fell from 115 to 93g. per day, while the consumption of carbohydrates rose from 395 to 429g. (13, p. 128)
They continued, “As fig. 4 shows (reproduced here as Figure 3), there is a close correlation between the curve for consumption of fat contained in these foods and the curve for mortality from circulatory diseases, with correction for age” (p. 128).
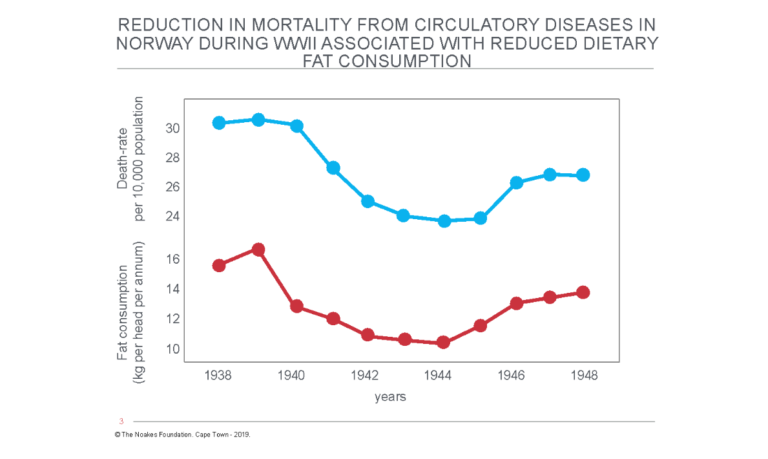
Figure 3: Dramatic reduction in mortality from circulatory diseases in Norway during World War II was associated with a reduction in total dietary fat consumption. Reproduced from reference 13.
Then Strom and Jensen added the proviso that would go missing once Keys took charge of the hypothesis: “We must, however, beware of regarding the evidence as decisive. Similar correlations could undoubtedly be demonstrated between mortality and trends in other commodities, such as sugar, coffee, tobacco, textiles, and footwear; yet the last two of these can hardly have exerted any influence on mortality” (p. 128, my emphasis).
Their parting comment is also instructive: “The war-time decline (in mortality) coincided with severe dietary restrictions. The supply of calories was reduced, and this reduction was principally of foods containing fat, including those rich in cholesterol” (p. 129, my emphasis).
John Gofman uses a novel technique
In August 1950, John Gofman, MD, published an iconic paper that had all the trappings of becoming a potential Nobel Prize winner (17). By exposing human blood to ultracentrifugation, which produces forces “many million times the force of gravity” (p. 162), he was able to identify a range of molecules of different densities, or in technical terms, different flotation rates, measured as different Svedberg (Sf) values. Thus, lower density lipoproteins such as chylomicrons and VLDL cholesterol (which Gofman was the first to identify and separate with this technique) have higher Sf values, and higher density lipoproteins such as LDL and HDL cholesterol have lower values.
Already in his 1950 paper, Gofman was able to show the following:
- Individuals of both genders with myocardial infarction displayed “a very high frequency of occurrence of Sf 10-20 molecules in the serum” (17, p. 170).
- The same finding was reported in persons with Type 2 diabetes mellitus (17); in those with angina pectoris (a symptom of advanced coronary artery atherosclerosis); and in other groups of patients known to be at increased risk for developing CHD (nephrotic syndrome, hypothyroidism, hypertension).
- There was “a general trend toward higher Sf 10-20 concentrations with higher serum cholesterol levels, but for any particular patient the analytic serum cholesterol level is of no value in predicting the concentration of Sf 10-20 molecules” (p. 174).
- Gofman and his colleagues therefore argued, “Assuming our hypothesis of the relationship of molecules of the Sf 10-20 class to atherosclerosis to be correct, all these observations taken together may reveal the difficulty in trying to establish any correlation of the analytic serum cholesterol levels with the presence or severity of atherosclerosis.”
- A single meal of fat and cholesterol did not influence the blood Sf concentrations.
- “There was no consistent relationship between the dietary cholesterol or fat intake and the blood level of Sf 10-20 molecules in the group as a whole. This would suggest that there is a wide range of individual tolerances to the usual levels of these substances in the diet” (p. 176).
- A group of patients who had been prescribed “a strict low fat and low cholesterol diet for periods of three months to three years … (had) lower concentration of molecules of the Sf 10-20 class than either normal or … other myocardial infarction patients of corresponding age and sex categories. This represents indirect supportive evidence of the efficiency of dietary restriction to reduce the concentration of the Sf 10-20 molecules in the serum” (p. 176-177).
In subsequent studies, Gofman extended the range of “atherogenic” lipoproteins to those with Sf values of 12-100 (19). He also came up with an Atherogenic Index (AI) based on the concentration of the Sf 0-12 and Sf 12-400 lipoproteins (22). In one study, he found the AI was elevated in persons with CHD and that AI could predict prognosis in patients with angina pectoris and after myocardial infarction.
Gofman and his co-authors argued AI was “much superior to the serum cholesterol measurement as an indicator of the lipid disorder in coronary disease” (p. 325). They also found the low-fat, low-cholesterol diet effectively maintained “chronically lowered lipoprotein AI values” (p. 325). They wrote, “In patients who said they did not adhere to a low fat, low cholesterol diet, the recurrence in death rate was four times as high as in [heart attack] patients who stated that they adhered to the diet” (p. 325).
So already in August 1950, Gofman had concluded Sf 10-20 molecules were overrepresented in person either with established CHD or at increased risk for its development; “the presence of these cholesterol-bearing lipid and lipoprotein molecules cannot be predicted from the analytic total serum cholesterol level” (p. 177); and “partial dietary restriction of fat and cholesterol in man results in a gradual decrease in the serum level of such molecules over a period of weeks or months” (p. 177). As a result, he and his colleagues proposed, “The presence of these molecules … supports the hypothesis of their association with atherosclerosis” (p. 177).
This is the foundation of what would become known as Keys’ diet-heart and lipid hypotheses — most of which had already been described three years before Keys’ first description of it.
Ancel Keys’ Damascene Moment
We return now to the story of how Keys, the original cholesterol denialist (7), would convert within a few years to someone who would “declare war on cholesterol” (23, p. 132).
Keys’ version of the story is that while attending a scientific conference on malnutrition in Rome in 1951, he was informed by Professor of Physiology at the University of Naples Dr. Gino Bergami that CHD was not a problem among the Neapolitan people (23, p. 16-17;17). The following year, Bergami invited Keys and his wife, Margaret, to Naples to come and see for themselves. Margaret Keys had a special scientific talent for measuring blood cholesterol concentrations.
In Naples, Ancel found, or at least convinced himself of the fact, that the working classes in Naples were indeed CHD-free. The same was not true of the wealthy:
‘I was taken to dine with members of the Rotary Club,’ Keys wrote. ‘The pasta was loaded with meat sauce and everyone added heaps of parmesan cheese. Roast beef was the main course. Dessert was a choice of ice cream or pasty. I persuaded a few of the diners to come for examination, and Margaret found their cholesterol levels were much higher than the workmen.’ Keys found ‘a similar picture’ when he visited Madrid. Rich people had more heart disease than poor people, and rich people ate more fat. (9, p. 17)
In his retelling of the story in 1994, Keys (24) mentioned the influence of the studies of Malmros and others on his thinking. He forgot that in 1952 he was quite dismissive of their work (25):
The recent analysis of mortality data in Scandinavia (11) is more acceptable but still suffers from the inherent weakness of attempting to discover causation from a parallelism between crude estimates of national averages for two variables. Besides the dubious point of attributing war-time changes in vital statistics to actual changes in atherosclerosis, the analysis glosses over the fact that the presumed variations in cholesterol intake were parallel to similar variations in total dietary fat intake and, at least to some extent, to changes in calorie intake and physical activity. (25, p. 115-116)
Perhaps he also did not remember writing this: “Now clearly the cholesterol level is not the whole story in the development of atherosclerosis” (25, p. 117).
Yet one year later, he would write, “Many factors are probably involved in the atherosclerotic development and in the clinical appearance of coronary heart disease, but there is no longer any doubt that one central item is the concentration, over time, of cholesterol and related lipids and lipoproteins in the blood serum. No other etiological influence of comparable importance is as yet identified” (26, p. 1399-1400, my emphasis).
And later in the same article:
Let us now return to the diet. There are enough good reasons to suspect that our present high-fat diet in the United States is scarcely favourable to the health of adult men, even though it is premature to blame it as the whole cause of our excessive mortality from heart disease. The changes in mortality in countries forced to alter their diets during the late World War cannot be ignored. These changes conform to the concept that the proportion of fat in the diet is closely related to the development of atherosclerotic heart disease (11-13). (p. 1405, my emphasis).
These historical statements are crucial to any understanding of how Keys first changed his own mind and then succeeded in convincing the rest of the world. They show that in 1952, Keys fully appreciated that associational studies like those performed by Malmros (11) and Strom and Jensen (13) cannot prove causation for all the reasons he described. At that time, he also concluded that blood cholesterol levels are “not the whole story” in the development of CHD.
Yet a year later, he had completely reversed his positions on both topics. In the absence of any new evidence, he then declared “there is no longer any doubt” that blood cholesterol (and other blood lipids) and high-fat diets are driving the development of coronary atherosclerosis. And the evidence he claimed was so important that it could no longer “be ignored” came from those same war-time studies that just one year earlier he had dismissed as incomplete because they were based on “crude” associational data that in any case could not prove causation.
I submit that he changed his mind so abruptly purely because he was at heart an opportunist who saw an opening too inviting to let go. He was too weak to resist the temptation, so he rushed through that open door.
The problem for the rest of the world was that once he had come up with his twin hypotheses (based on circumstantial evidence that he clearly understood could never prove causation), Keys would not give up on them. Instead, he began to exhibit the signs and symptoms of a common scientific ailment: He fell in love with his hypotheses and convinced himself he had discovered a universal truth. He continued to defend his hypotheses with all his might for the rest of his long earthly life, dying just short of his 101st birthday.
So how did Keys convince himself and then the world that his hypotheses, beginning with such flimsy evidence and amid so many other credible and competing explanations, should be accepted as truth?
Keys uses weak epidemiological evidence
Since we now know Keys did not begin his research with any preconception that one particular dietary substance was the cause of the CHD epidemic, something drastic had to happen to change his mind between 1949 and 1953 when he published his original paper describing the diet-heart hypothesis. Surely, it could not just have been the result of attending the Rotary Club dinner in Naples in 1952, or even the circumstantial evidence showing the reduction in CHD mortality in some countries during WWII (11-14)? Surely there must have been some indisputable evidence from his or others’ research, the results of which had already been published by 1953? Well, of course, there was Gofman’s work. But Keys was spectacularly dismissive of Gofman’s work — even though his conclusions in his first major 1953 description of his hypotheses became the mirror image (8) of everything Gofman had already presented in his 1950 paper (17).
Keys’ first scientific study of 281 Minnesota business and professional men (MBPM) began in 1947 at a time when Keys did not apparently believe a dietary factor was a likely cause of coronary heart disease. The study lasted 15 years and was funded jointly by the U.S. Public Health Service (presumably through the Heart Institute) and the American Heart Association (AHA). The results were first published in 1962 (6). Thus the results of that study could not have informed Keys’ opinion in 1953.
The major finding of the study was that 32 of the original 281 study subjects who developed “definite” coronary heart disease had higher blood cholesterol concentrations than those who did not develop any symptoms of heart disease. Yet 14 of those 32 (44%) had below normal blood cholesterol concentrations. Men who developed heart disease despite low blood cholesterol concentrations were more likely to be hypertensive and overweight. Despite this, the study concluded blood cholesterol concentration was the sole predictor of future heart attack risk.
But Keys would only know this evidence for certain in 1962, long after he had already become convinced that saturated fat was the dietary villain; and seven years after Eisenhower’s heart attack in 1955.
Importantly, the MBPM study did not include any measure of what the subjects ate. This is presumably because when Keys planned the study in 1947, he did not yet believe diet played any specific role in heart disease. So why would he have designed a study in 1947 to measure the effects of diet on the future development of CHD? The fact that he did not is a missing piece of evidence science historians may have overlooked.
The only evidence Keys had in 1955, when White placed President Eisenhower on Keys’ experimental and untested diet, was his 1953 paper (8).
Crucially, that paper did not include any novel data Keys had personally collected from studies of patients with established coronary heart disease — data that would have convinced him then, or should convince us now, that he had reason to change his mind so radically.
Instead, he presented a wide range of circumstantial evidence from many different sources to formulate what would become known as his diet-heart and lipid hypotheses: He began to argue a diet high in saturated fat from animal sources causes heart disease by increasing the blood cholesterol concentration (diet-heart hypothesis), and the elevated blood cholesterol concentration then forces cholesterol to enter from the bloodstream into the walls of the coronary arteries, producing coronary atherosclerosis (Iipid hypothesis).
Reading that paper with the benefit of 66 years of hindsight shows that even though he did not have any definitive proof for his theories, Keys appeared to be absolutely certain he was correct. I am left to conclude that the reason Keys went from being a cholesterol/saturated fat denialist in 1949 (7) to the opposite position in 1953 (8, 25-28) was not because he suddenly discovered irrefutable proof for these new ideas in that three-year period. It is clear there was no such irrefutable proof available at the time (as remains the case today (29, 30)). Even Gofman’s work can be classified as hypothesis-generating, not as conclusive. Certainly, as I shall relate, the “evidence” Keys presented was too weak, too circumstantial, and too contradictory ever to prove his case.
In any case we know that in 1952, he clearly appreciated the “inherent weakness of attempting to discover causation from a parallelism between crude estimates of national averages for two variables” (25, p. 115). Yet the major study he would initiate, the Seven Countries Study (SCS) (28), attempted to do just that.
As a result, that study could never produce the smoking gun that proved his ideas were irrefutably correct. In fact, as I will show, when he did finally design a study that could have provided the smoking-gun evidence for which he was searching, he discovered the opposite: He discovered evidence that irrefutably proved both his hypotheses were completely wrong.
And faced with that inconvenient truth, the opportunist did what came naturally. He hid the evidence in the hope that no one would ever find it.
Unfortunately for Keys, that truth was finally exposed (33).
Inherent Flaws Found in Keys’ So-Called Facts
In his first major iteration of his newly minted hypotheses in 1953, Keys presented what he considered to be four basic but unrelated facts (8, p. 122):
1) It is a fact that, compared with healthy persons of the same age, patients with definite angina pectoris or who have survived a myocardial infarction tend to have blood serum characterized by high cholesterol and certain lipoprotein concentrations, a high cholesterol-phospholipid ratio, and a larger proportion of the cholesterol in the beta lipoprotein fraction.
2) It is a fact that, on the average, persons afflicted with diabetes, myxedema and nephrosis tend to have high cholesterol and the other peculiarities mentioned above. Among these patients there is a high incidence of atherosclerosis and degenerative heart disease.
3) It is a fact that in animal experiments those measures, such as high cholesterol diets and thyroid suppression, which produce high levels of cholesterol and allied substances in the serum, are also productive of atherosclerosis.
4) It is a fact that a major characteristic of the atherosclerotic artery is the presence of abnormal amounts of cholesterol in that artery. The atherosclerotic plaque consists of 40 to 70 per cent cholesterol. It is extremely probable that most or all of this cholesterol is derived from the blood. The cholesterol in the blood does not exist as a simple solution of free and ester cholesterol; it is carried in lipoprotein complexes. (8, p. 122, my emphasis).
In his 1953 paper, he relegates references to the change in mortality associated with dietary changes in certain countries during WWII to a single paragraph and does not discuss how this influenced his thinking. And he mentions the work of Gofman only to criticize and dismiss it as essentially irrelevant (31, 32).
From all this highly circumstantial evidence, he argued, “All of this indicates that measurement of cholesterol and allied substances in the blood serum affords an indication of the tendency towards the development of atherosclerosis and degenerative heart disease” (p. 122, my emphasis). He added, “Other things being equal, there seems to be no doubt that high serum levels of cholesterol, etc., are undesirable and the higher the values the more undesirable they are. Hence there is every justification for devoting great effort to discovering what determines the level in man and how that level may be controlled” (p. 125, my emphasis).
But Keys presented no incontrovertible proof to support these conclusions. He quite simply presented a convoluted concoction of circumstantial evidence that advanced an untested hypothesis as if it was already a proven fact. In part, Keys was likely able to achieve this because of the force of his character and his Svengali-like ability to convert the strong, mighty, and influential — including Paul Dudley White and later President Eisenhower — to believe his hypothesis was as good as proven fact, even in the absence of proof.
The key piece of novel “evidence” presented in the 1953 paper is the graph reproduced in Figure 4. Note the figure does not include any reference to blood cholesterol concentrations and thus does not address the lipid hypothesis. This figure would launch Keys’ diet-heart hypothesis.
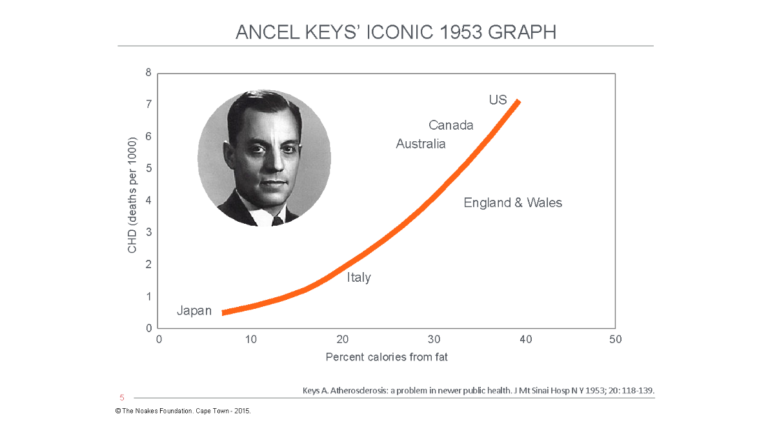
Figure 4: In his 1953 paper (8), Keys included data from six countries, apparently showing a close relationship between the increasing percentage of fat in the diet (as a percentage of total calories) and deaths per 1,000 persons from degenerative (atherosclerotic) heart disease. He hypothesized that this (associational) relationship could be explained by higher blood cholesterol concentrations in persons living in countries ingesting more dietary fat, as in the U.S., Canada, and Australia. The patent flaws in Keys’ argument were ruthlessly exposed by Jacob Yerushalmy and Herman Hilleboe in 1957 (33). In particular, they emphasized that findings from epidemiological (associational) studies cannot prove causation except in uniquely exceptional circumstances these data did not fulfill. Reproduced from reference 8.
Keys’ principal conclusion from this graph was, “Whether or not cholesterol, etc., are involved, it must be concluded that dietary fat somehow is associated with cardiac disease mortality, at least in middle age” (p. 134, my emphasis).
This is perhaps the first example of how Keys would, throughout his scientific life, continuously confuse hypothesis and proven theory. The final conclusion he drew goes far beyond the weak associational epidemiological evidence he had presented: “The concentration of total cholesterol in the blood serum bears an important relationship to the development of atherosclerosis and its sequelae and related conditions. Similar relationships exist with the concentrations of certain ‘giant molecules’ (Sf 10-20, Sf 12-20) and of certain lipoprotein fractions” (p. 136, my emphasis).
Yet Keys provided no direct evidence to support such a conclusion. Nowhere in Figure 4 is there any mention of blood cholesterol concentrations or of “giant molecules.” And he only provided weak “evidence” for that relationship in his next paper (20), published four years later. The conclusion to his 1953 paper simply stated what must be true if his hypothesis was to survive (8).
But there is a more disturbing feature of this paper (8), which until now has gone unnoticed, and that is Keys’ clear attempt to minimize the contributions of Gofman. Keys did this by initially discrediting Gofman’s findings, concluding the ultracentrifugation technique for measurement of blood lipoprotein Sf fractions did not add value for predicting who was likely to develop CHD. Significantly, however, Keys then contradicted himself by reproducing most of the conclusions Gofman had already made (17-19). He, of course, neglected to adequately acknowledge Gofman’s contributions, and in fact, Keys’ actions appear to border on plagiarism. Regardless, Keys’ tactics effectively wrote Gofman out of history and presented Gofman’s work as if it had been made by Keys. Keys, the false scientist, had successfully seized the scientific high ground from perhaps the most highly qualified scientist in the field.
Thus, Keys wrote the following:
- “The concentration of total cholesterol in the blood serum bears an important relationship to the development of atherosclerosis and its sequelae and related clinical conditions. Similar relationships exist with the concentrations of certain “giant molecules” (Sf 10-20, Sf 12-20) and of certain lipoprotein fractions separable by precipitation methods” (p. 136). [Note: Having gone out of his way in 1951 (31, 32) to minimize the relevance of Gofman’s novel finding as “entirely unjustified to attribute to G(iant) measurements any special virtue beyond that of simple cholesterol measurements for the prediction of atherosclerosis or the estimation of the activity of the atherosclerotic process” (31, p. 473), Keys then sought to claim credit for this finding.]
- “Measurement of total cholesterol and of Sf 12-20 particles in the serum afford highly significant differentiation between groups of men who are clinically healthy and groups of men who are likely to develop coronary heart disease” (p. 136). [Note: This finding is exactly as Gofman reported it (17). Keys made no mention of the origin of this finding.]
- “The total cholesterol concentration in the serum of men habitually on diets characteristic of the United States changes directly with changes in the total fat content of the diet” (p. 136). [Note: This is exactly as Gofman had described it (17). Again, Keys made no acknowledgement of his source.]
Then, Keys concluded the article with another important statement that has gone largely unnoticed: “The measurements of total cholesterol or of Sf concentrations in the serum have very little practical value for individual diagnosis or prognosis” (p. 136). This statement conflicts absolutely with the one speculation he wanted us all to accept uncritically: “The concentration of total cholesterol in the blood serum bears an important relationship to the development of atherosclerosis and its sequelae and related conditions” (p. 136).
If blood cholesterol concentrations cannot differentiate between those who will and will not develop CHD, then how can cholesterol be driving the atherosclerotic process according to Keys’ lipid hypothesis?
The source of Keys’ information for his iconic figure
The truth is that after Keys had experienced his Damascene moment in Naples in 1952, he likely realized that, to secure a steady supply of continuous funding from the treasure trove controlled by the NHI, he urgently needed to find evidence to convince funders to support him. He needed something, anything, no matter how quick and dirty, to get the jump on his competitors — especially Gofman, who by 1952 had already published three papers describing the diet-heart and lipid hypotheses (17-19).
Waiting 10 to 15 years for the initial findings from the Minnesota Business and Professional Men’s Study (6) was not the solution. And what if the results were unfavorable? No, he needed evidence, from whatever source, that would clearly support his theory.
He found his solution in a 1953 publication of the World Health Organization (WHO) Annual Epidemics and Vital Statistics (34, p. 6; 33, p. 923). There, he found the information shown graphically in Figure 5. We call this type of research “armchair” science. The scientist does not need to move from the comfort of the easy chair in his living room to collect the information.
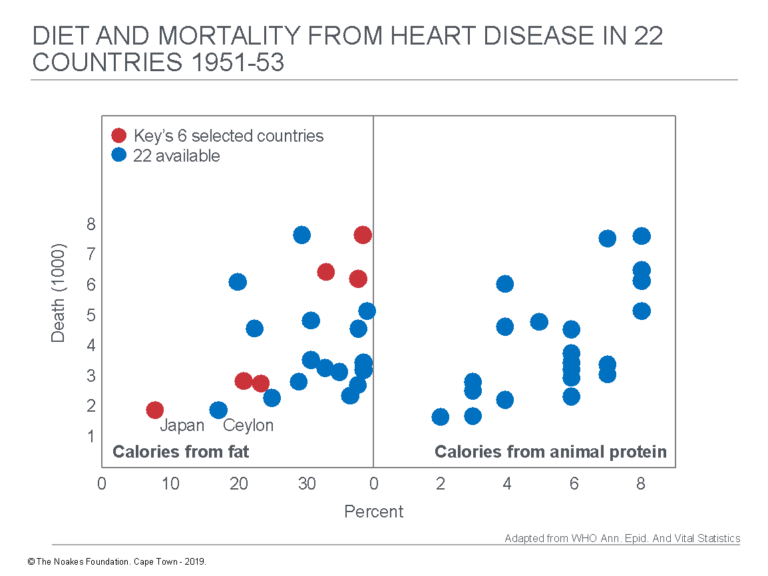
Figure 5: The data Keys sourced to draw up his famous 1953 figure came from an annual publication produced by the WHO. The left panel in this figure shows the data for annual death rates versus calories from dietary fat for 22 countries for which data were then available. Keys selected just six of those countries (red dots) and excluded the remainder (blue dots). The right panel shows the relationship between death rates and calories from animal protein. Keys did not report this information. Reproduced from reference 34, p. 6; 35 p. 923).
Simple visual analysis of Figure 5 suggests the data in the right panel — calories from animal protein — show at least as good a correlation with annual death rates as do calories from fat (left panel). Yet Keys never presented any evidence linking “calories from animal protein” to rates of heart disease. So why did he focus exclusively on “calories from fat” and ignore “calories from animal protein”?
As I will discuss in the next column, Yerushalmy and Hilleboe (33) would confirm the suspicions that arise from the visual impression. They showed animal protein intake had a statistically closer relationship with annual heart disease death rates than did fat intake.
The left panel in Figure 5 is the best evidence there could be that Keys “cherry-picked” the six countries (from 22) that would give him the “evidence” he wanted. He clearly had devious intent. Why else would he have chosen those six specific countries that fit so neatly on his published graph (Figure1)? Given the extent of the havoc his choice would visit on the world, did he act recklessly? Mann’s opinion is clear: “Such data selection is, of course, cheating” (34, p. 6).
As a result of this devious action, Keys’ hypothesis that dietary fat was the single most important cause of CHD was up and running. Any possibility that there might be other, better explanations for CHD causation had already been effectively marginalized and would remain so for at least the next seven decades — right up to the present.
Additional Reading
- It’s the Insulin Resistance, Stupid: Part 1
- It’s the Insulin Resistance, Stupid: Part 2
- It’s the Insulin Resistance, Stupid: Part 3
- It’s the Insulin Resistance, Stupid: Part 4
- It’s the Insulin Resistance, Stupid: Part 5
Professor T.D. Noakes (OMS, MBChB, MD, D.Sc., Ph.D.[hc], FACSM, [hon] FFSEM UK, [hon] FFSEM Ire) studied at the University of Cape Town (UCT), obtaining a MBChB degree and an MD and DSc (Med) in Exercise Science. He is now an Emeritus Professor at UCT, following his retirement from the Research Unit of Exercise Science and Sports Medicine. In 1995, he was a co-founder of the now-prestigious Sports Science Institute of South Africa (SSISA). He has been rated an A1 scientist by the National Research Foundation of SA (NRF) for a second five-year term. In 2008, he received the Order of Mapungubwe, Silver, from the President of South Africa for his “excellent contribution in the field of sports and the science of physical exercise.”
Noakes has published more than 750 scientific books and articles. He has been cited more than 16,000 times in scientific literature and has an H-index of 71. He has won numerous awards over the years and made himself available on many editorial boards. He has authored many books, including Lore of Running (4th Edition), considered to be the “bible” for runners; his autobiography, Challenging Beliefs: Memoirs of a Career; Waterlogged: The Serious Problem of Overhydration in Endurance Sports (in 2012); and The Real Meal Revolution (in 2013).
Following the publication of the best-selling The Real Meal Revolution, he founded The Noakes Foundation, the focus of which is to support high quality research of the low-carbohydrate, high-fat diet, especially for those with insulin resistance.
He is highly acclaimed in his field and, at age 67, still is physically active, taking part in races up to 21 km as well as regular CrossFit training.
REFERENCES
- Keys A, Keys M. Eat Well and Stay Well. Garden City, NY: Doubleday and Company, Inc., 1963.
- Noakes TD. It’s the insulin resistance, stupid: Part 5. CrossFit.com. 22 Oct. 2019. Available here.
- White PD. Heart Disease, 3rd ed. New York, NY: The Macmillan Company, 1946.
- Keys A, Brozek J, Henschel A, et al. The Biology of Human Starvation. Minneapolis, MN: University of Minnesota Press, 1950.
- Olszewski TM. The causal conundrum: The diet-heart debates and the management of uncertainty in American Medicine. J Hist Med Allied Sci 70(2014): 218-249.
- Keys A, Taylor HL, Blackburn H, et al. Coronary heart disease among Minnesota business and professional men followed fifteen years. Circulation 28(1962): 381-394.
- Smalley A. St. Paul Pioneer Press, October 11, 1949. In: Henry Blackburn reviews 1938-1955 albums of Laboratory of Physiological Hygiene news reports as now preserved on CDs in the Division of Epidemiology and in University Archives. Available here.
- Keys A. Atherosclerosis: A problem in newer public health. J Mt Sinai Hosp 20(1953): 118-139.
- Taubes G. Good Calories, Bad Calories: Fats, Carbs, and the Controversial Science of Diet and Health. New York: NY: Anchor Books, 2008.
- Keys A, Anderson JT. The relationship of the diet to the development of atherosclerosis in man. In: Symposium on atherosclerosis. National Academy of Sciences – National Research Council Publication 338. Washington, D.C.: 1954. pp. 181-197.
- Malmros H. The relation of nutrition to health. A statistical study of the effects of the war-time on arteriosclerosis, cardiosclerosis, tuberculosis and diabetes. Acta Med Scand Suppl 246(1950): 137-53.
- Pihl A. Cholesterol studies. II. Dietary cholesterol and atherosclerosis. Scan J Clin Lab Invest 4(1954): 122-133.
- Strom A, Jensen AR. Mortality from circulatory diseases in Norway 1940-45. Lancet 260(1951): 126-129.
- Henschen F. Geographic and historical pathology of arteriosclerosis. J Gerontol 8(1953): 1-5.
- Strom A. Examination of the diet of Norwegian families during the war years 1942-1945. Acta Med Scand 131 suppl. 214(1948): 1-47.
- Vartainen I, Kanerva K. Arteriosclerosis and war-time. Ann Med Intern Fenn 36(1947): 748-758.
- Gofman JW, Jones HB, Lindgren FT, et al. Blood lipids and human atherosclerosis. JAMA 11(1950): 161-178.
- Jones HB, Gofman JW, Lindgren FT, et al. Lipoproteins in atherosclerosis. Am J Med 11(1951): 358-380.
- Gofman JW. Diet and lipotrophic agents in atherosclerosis. Bull NY Acad Med 28(1952): 279-293.
- Gofman JW, Glazier F, Tamplin A, et al. Lipoproteins, coronary heart disease and atherosclerosis. Physiol Rev 34(1954): 598-607.
- Gofman JW, Tamplin A, Strisower B. Relation of fat intake to atherosclerosis. J Am Diet Assoc 30(1954): 317-326.
- Lyon TP, Yankley A, Gofman GW, et al. Lipoproteins and diet in coronary heart disease. A five-year study. Cal Med 84(1956): 325-328.
- Levenstein H. Fear of Food: A History of Why We Worry About What We Eat. London, U.K.: University of Chicago Press, 2012.
- Keys A. The inception and pilot surveys. In: Kromhout D, Menotti A, Blackburn H. The Seven Countries Study: A Scientific Adventure in Cardiovascular Disease Epidemiology. Marjan Nijssen-Kramer, Bilthoven, Netherlands: Studio RIVM, 1993. pp. 15-25. Available here.
- Keys A. Human atherosclerosis and the diet. Circulation 5(1952): 115-118.
- Keys A. Prediction and possible prevention of coronary disease. Am J Publ Health 1953: 1399-1407.
- Keys A, Grande F. Role of dietary fat in human nutrition. III – Diet and the epidemiology of coronary heart disease. Am J Pub Health 47(1957): 1520-1530.
- Kromhout D, Menotti A, Blackburn H. The Seven Countries Study: A Scientific Adventure in Cardiovascular Disease Epidemiology. Marjan Nijssen-Kramer, Bilthoven, Netherlands: Studio RIVM, 1993. Available here.
- Teicholz N. The Big Fat Surprise: Why Butter, Meat and Cheese Belong in a Heathy Diet. New York, NY: Simon and Schuster, 2014.
- Harcombe Z. An Examination of the Randomized Controlled Trials and Epidemiological Evidence for the Introduction of Dietary Fat Recommendations in 1977 and 1984: A Systematic Review and Meta-Analysis. University of West Scotland, March 2016.
- Keys A. “Giant molecules” and cholesterol in relation to atherosclerosis. Bull J Hopkins Hosp 88(1951): 473-483.
- Keys A. Cholesterol, “Giant molecules” and atherosclerosis. JAMA 147(1951): 1514-1519.
- Yerushalmy J, Hilleboe HE. Fat in the diet and mortality from heart disease. A methodological note. New Y State J Med 57(1957): 2343-2354.
- Mann GV. A short history of the diet/heart hypothesis. In: Coronary Heart Disease: The Dietary Sense and Nonsense. An Evaluation by Scientists. London, England: Janus Publishing Company, 1993. pp. 1-17.