This 2018 review summarizes links between metabolic syndrome, insulin resistance, and Alzheimer’s disease.
Observational evidence increasingly shows diabetes, obesity, and other forms of metabolic disease are linked to increased risk of Alzheimer’s disease (1), and that patients with Alzheimer’s disease are more likely to be insulin-resistant than peers who do not have the disease (2). Insulin action in the brain promotes synaptic plasticity and memory formation, all of which are impaired in the brains of patients with Alzheimer’s (3). Decreased brain insulin and IGF signaling have themselves been directly correlated with Alzheimer’s disease risk and severity, with brains of patients with Alzheimer’s showing reduced activation of insulin, IGF, PI3K, and Akt-related pathways (4). Reduced cerebral IRS-1 signaling may appear as much as a decade prior to the visible effects of Alzheimer’s, which suggests insulin resistance may contribute to the disease’s cause or progression (5). Additionally, drugs that improve insulin signaling, such as certain antidiabetic drugs and intranasal insulin, have been shown in some preliminary research to reduce Alzheimer’s risk and/or reduce symptom severity (6).
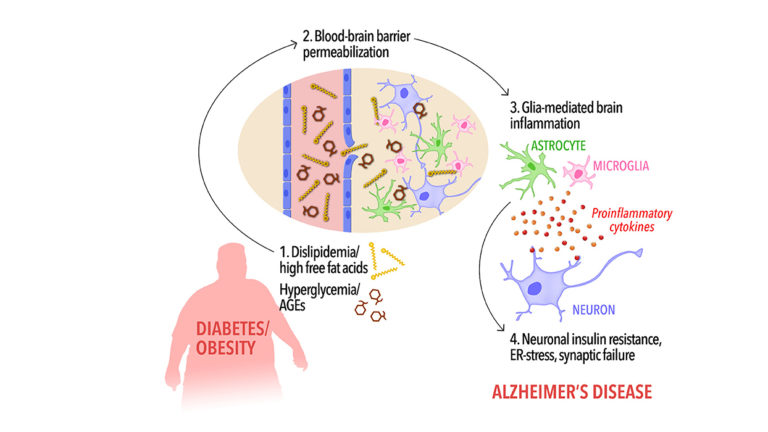
The mechanism by which metabolic disease can reduce brain insulin signaling is not precisely known, as discussed recently on CrossFit.com. These researchers, however, noted insulin-resistance-associated changes in the composition of circulating fatty acids may increase the permeability of the blood-brain barrier to inflammatory cytokines and other factors that impair insulin signaling in CNS cells. Future research is needed to understand how the various changes associated with metabolic disease individually and collectively contribute to reduced CNS insulin signaling.
In sum, the research surveyed here is insufficient to support a direct cause-and-effect relationship between metabolic disease (obesity, diabetes, and the metabolic syndrome) and Alzheimer’s disease, but the correlation is consistent with a causal relationship.
Notes
- Glucose levels and risk of dementia; The Rotterdam Study: 2018 update on objectives, design and main results; Insulin resistance and alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes; Obesity, abdominal obesity and Alzheimer disease
- Demonstrated brain insulin resistance in Ahzleimer’s disease patients is associated with IGF-1 resistance, IRS-1 dysregulation and cognitive decline; Alzheimer’s disease and insulin resistance: Translating basic science into clinical applications
- Brain insulin resistance in type 2 diabetes and Alzheimer disease: Concepts and conundrums; Insulin resistance is associated with the pathology of Alzheimer disease: The Hisayama study
- Insulin dose-response effects on memory and plasma amyloid precursor protein in Alzheimer’s disease: Interactions with apolipoprotein E genotype; The effect of insulin and glucose on the plasma concentration of Alzheimer’s amyloid precursor protein; Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer’s disease – Is this type 3 diabetes?; An anti-diabetes agent protects the mouse brain from defective insulin signaling caused by Alzheimer’s disease- associated Aβ oligomers
- Dysfunctionally phosphorylated type 1 insulin receptor substrate in neural-derived blood exosomes of preclinical Alzheimer’s disease
- Sniffing neuropeptides: A transnasal approach to the human brain; Safety of intranasal human insulin; To target the human brain in disease and health
Comments on Insulin Resistance in Alzheimer's Disease
When you consider that the NIH estimates that the cost of dealing with Alzheimer's Disease in the next 30 years could top $1.5 trillion (with a 't') the need for addressing it is self-evident, separate and apart from the incalculable human costs borne by the sufferers and their families. Big Pharma is on the case, of course, searching for some magic, patentable medication to treat it once it's declared itself. But if the connection proves out (as it looks like it should) that Alzheimer's is basically another dark star in the insulin resistance constellation, then addressing it by the same means as you would/should address diabetes or any other of the IR panoply of symptoms--e.g., through a decent whole food diet, replete with good quality (animal) protein from meat, fish, poultry, game, eggs, and dairy, fresh low-starch veggies and low-sugar fruits, nuts and seeds, and plenty of good fats and devoid of industrial seed oils, sugar and refined starches--seems like a promising and cost-effective option. The brain is mainly fat and it needs fat and dietary cholesterol to thrive. Starving it of these critical nutrients in the name of lowering LDL to prevent heart disease (which while erroneous has long been the purported reason to avoid animal fats and replace them with so-called 'heart healthy', 'vegetable' fats) is to my mind a blatant and callous violation of the foundational pillar of the Hippocratic Oath: first, do no harm.
Insulin Resistance in Alzheimer's Disease
1