In the 1960s, researchers noticed the Inuit, who consumed large amounts of omega-3 fats, experienced low rates of myocardial infarction. This observation led to the hypothesis that perhaps these particular polyunsaturated fats offered some sort of protection against heart disease. The authors of this 2015 review contribute to the still growing body of medical literature on the topic with their speculations regarding the effectiveness of omega-3 fats and their metabolites as protective agents against the development of cardiovascular disease.
Sixty plus years of research have uncovered an array of ways omega-3 fats might reduce the risk of heart attack and other cardiovascular diseases.
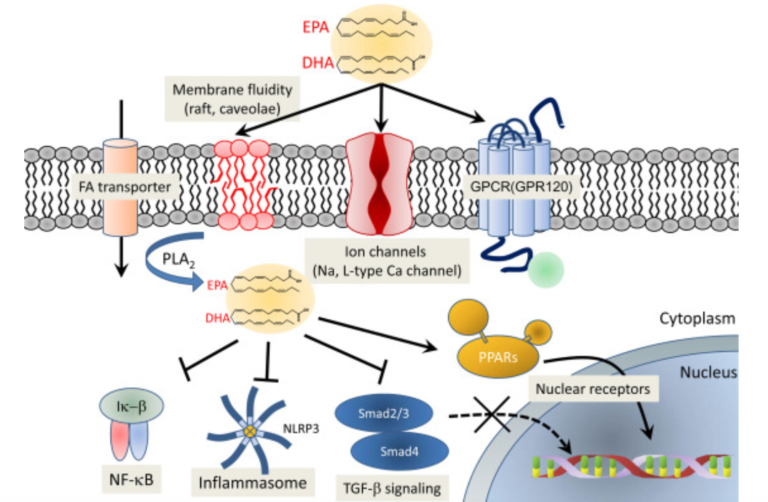
One of the primary ways is through their modulation of the electrophysiology of the cardiomyocytes. They do this by becoming incorporated into the phospholipid bilayer, where they can control the membrane ion channels, increasing the threshold for membrane depolarization. They also modulate the activity of calcium channels. Both effects decrease the chance of lethal arrhythmias.
Omega-3 fats also include many anti-inflammatory properties, which can serve to modify NF-kB signaling, suppress the NLRP3 inflammasome, and inhibit the operation of a handful of other inflammatory mediators.
The long-chain omega-3 fats eicosapentanoic acid (EPA) and docosahexanoic acid (DHA) also work through another inflammation-reducing pathway by preventing the conversion of arachidonic acid (AA) into the pro-inflammatory mediators prostaglandin E2 and leukotriene B4. These fats have the ability to serve as the substrate for prostaglandin E3 and leukotriene B5, which are much less inflammatory.
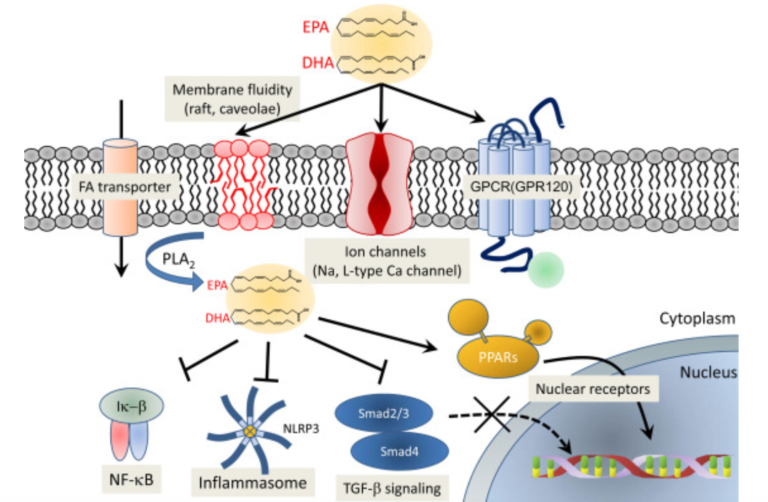
Figure 1: The proposed molecular mechanism of cardioprotection by omega-3 PUFAs
Not only do EPA and DHA reduce inflammation by blocking the products of AA, they also reduce inflammation directly by converting to specialized pro-resolving mediators (SPMs). SPMs — resolvins, protectins, and maresins — derive from omega-3 fats and exert their anti-inflammatory effects in a host of different ways. In addition to reducing inflammation, SPMs support cardiovascular health by protecting against brain ischemia, renal ischemia, reperfusion injury, insulin resistance, and atherosclerosis.
Other EPA and DHA metabolites — PGI3 and TXA3 — have anti-platelet effects and reduce platelet aggregation.
The authors point out that since atherosclerosis is recognized as an unresolved inflammatory disease involving the vascular wall, it is “assumed that the pathogenesis of atherosclerosis involves a decrease in SPM production.” This, of course, leads to the assumption that SPM replacement, through the agency of increased dietary omega-3 intake, might “control the local inflammatory response and improve the atherosclerotic changes.” There is data showing that in addition to preventing cardiac ischemia/reperfusion injury, SPMs deploy a number of direct cardioprotective actions, attenuating experimental infarct size and accelerating the resolution of the acute inflammation following myocardial infarction.
Using a transgenic mouse model — the Fat-1 mouse — these authors identified “a novel anti-inflammatory and anti-fibrotic EPA metabolite, 18-HEPE.” The Fat-1 mouse includes an encoded desaturase gene that converts omega-6 fats to omega-3 fats. This means these mice have enriched omega-3 fats in almost all tissues. Consequently, they were resistant to “numerous inflammatory diseases, including colitis, pancreatitis, osteoarthritis, atherosclerosis, obesity-linked insulin resistance, and some cancers.” Furthermore, via the mechanism of omega-3-enriched macrophages, there was an anti-fibrotic effect in Fat-1 mice subjected to pressure overload. These mice exhibited resistance to pressure-overload-induced inflammation and fibrosis, as well as reduced cardiac function. The implication of the findings in this mouse model is that more dietary omega-3 fat versus omega-6 fats might help prevent those diseases.