The vasa vasorum (VV) — “vessels on vessels” — are blood vessels located on the outside of arteries (Figure 1). Arteries are living tissue and, like all cells, require blood flow to acquire nutrients and dispose of waste. When arteries are thin, they can get all the nutrients they need simply through diffusion from the arterial lumen (i.e., the center of the artery, which blood flows through). As the vessel thickens, this diffusion eventually becomes insufficient to reach the outermost cells. These outermost cells become hypoxic — that is, they suffer from an insufficient supply of oxygen, as well as other nutrients. To compensate, the VV develop, carrying blood from further up the artery or adjacent arteries and veins to provide a blood supply to these outermost cells. As hypoxia expands throughout the artery (a consequence of further thickening), the VV branch out from single vessels to networks (Figure 2).
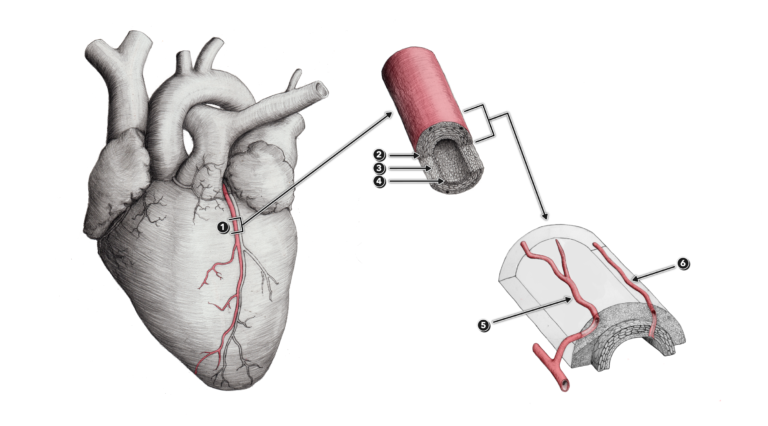
Figure 1
1 – Coronary artery
2 – Tunica externa (or tunica adventitia)
3 – Tunica media
4 – Tunica interna
5 – Vasa vasorum arising externally from a contributory artery or arteriole
6 – Vasa vasorum arising internally from the coronary artery itself
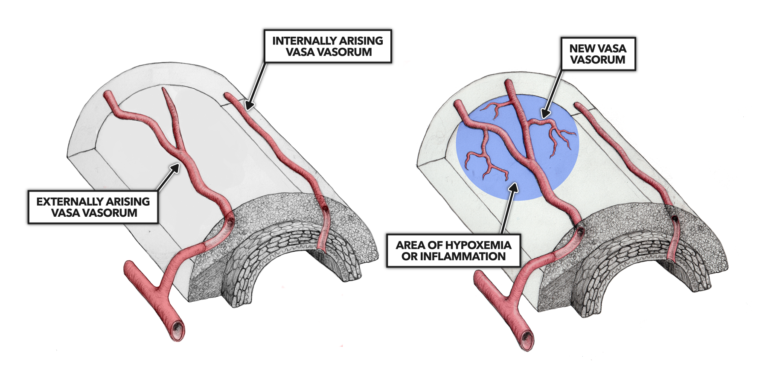
Figure 2
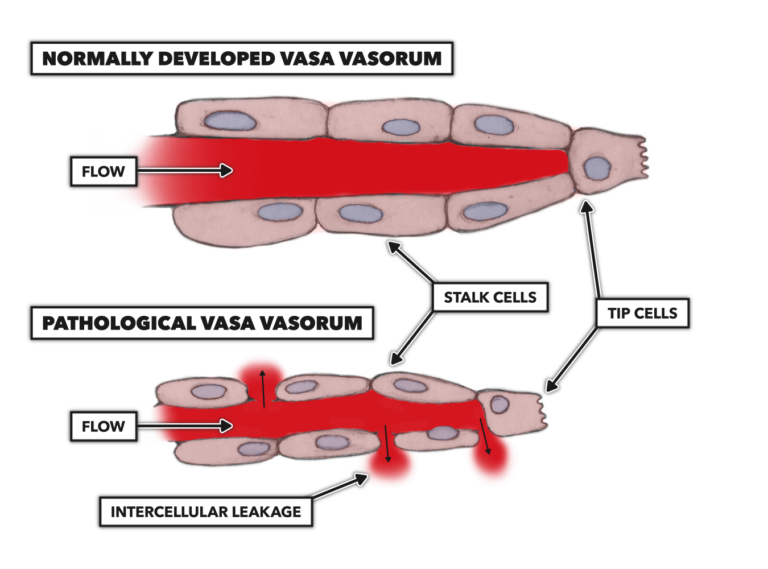
While these VV networks are a necessary adaptation to arterial thickening, they also increase the vulnerability of the arteries. VV, particularly as they branch into smaller vessels, are susceptible to degradation, leakage, and blockage. When this occurs, the VV can begin to leak pathogenic molecules — including lipoproteins, macrophages, infectious agents, and the other materials we observe within atherosclerotic plaques — from the bloodstream into the arterial walls (Figure 3).
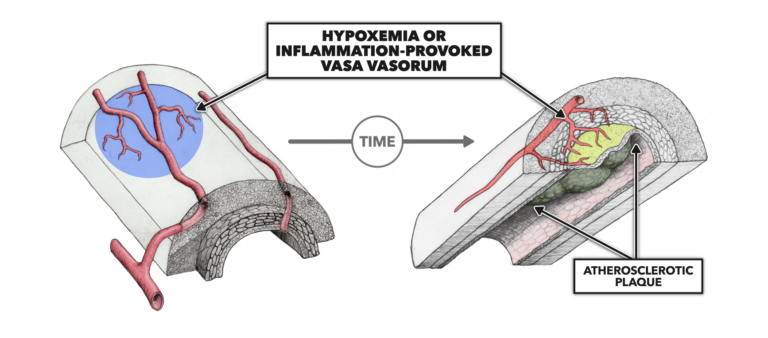
Figure 4
A small but interesting body of evidence suggests this damage to the VV may be the origin of atherosclerotic plaques (Figure 4). If this were the case, it would suggest lipid accumulation in arterial walls may increase the risk of plaque formation but is not the primary cause of plaque formation. Instead, that cause is damage to the VV. We will explore this hypothesis in future posts.
Comments on The Vasa Vasorum
Interesting hypothesis to explore and have more knowledge and option to cure heart diseases.
My wife suffered from a SCAD (spontaneous coronary artery dissection) 2+ years back and we're still no wiser today what caused it - she was perfectly healthy otherwise.
Until now I've never read anything which discusses arterial health or the impact of vessels on vessels. Such an interesting post for me because it's helped me to appreciate the massive complexity involved and why a cause and diagnosis may not be so simple.
Two key points 1. The effect is not the cause. Don’t confuse them. 2. Fats do not cause arterial disease. Bandaids don’t cause cuts. It’s easy to spot a cut with a bandaid, but it didn’t cause the cut. Nathan your comment is very interesting about the VV and hemodynamics and circulating pro inflammatory dietary factors.
Thanks Shakha! Very interesting topic and again, very glad to see it being addressed here on crossfit.com. This website is becoming my go-to resource for current scientific content.
Oh, and I think/hope it was clear from my initial comment that I am in no way questioning the main idea that fats/cholesterol do not cause atherosclerosis. I think that's been pretty well ruled out. Elevations in LDL-C are only observed in what, 50% of MI cases? And only about 30% of MIs are associated with occlusive atherosclerosis anyway.
The question that seems to remain open for investigation by 'real science' (as opposed to consensus science) is, what are the causal factors? A hypothesis is that the VV and hemodynamic signals interact to promote inflammation and atherosclerosis. Oxidative stress induced by poor diet is probably also required.
The key to the hypothesis that damage to the vasa vasorum drives the development of atherosclerotic plaque resides in the finding that the tunica intima is vastly more than one cell thick. I was taught in medical school that the intima was composed of a one-cell layer of endothelium, which would be very delicate. These cells were nourished by the blood flow within the lumen of the artery. Too much LDL-cholesterol carried by the blood flowing within the artery could invade this single-cell barrier, accumulate under the tunica intima, form a fatty streak, and, with continued accumulation, become plaque.
According to histograms I’ve seen published, during normal growth and development the intima grows from perhaps a single cell layer at birth to a size greater than the tunica media, the muscular layer of the artery, by early adulthood. Since the cells deep within this larger intima cannot be nourished by the simple diffusion from the blood coursing through the arteries, another method of feeding these cells has to develop. The vasa vasorum grows from within the deeper layers of the blood vessel to provide sustenance for these intimal cells. If plaque is to develop beneath the intima, the agents creating it must somehow depend on the vasa vasorum to get there. Simple diffusion won’t work.
An understanding of the microvascular anatomy, physiology, and pathology described above at the very least renders suspect the current dogma about the development of coronary plaque, i.e., that LDL-cholesterol slips beneath the intima causing endothelial dysfunction, inflammation, and plaque formation. By this theory high levels of LDL-cholesterol hasten the process, thus the near universal prescription to lower LDL-cholesterol to prevent and/or treat heart disease.
As the French physiologist Claude Bernard wrote:
“Indeed, proof that a given condition always precedes or accompanies a phenomenon does not warrant concluding with certainty that a given condition is the immediate cause of that phenomenon. It must still be established that when this condition is removed, the phenomenon will no longer appear…”
And as another researcher, W. E. Stehbens adds from a 1985 paper:
“. . . differentiating between cause and non-causative factors is essential. Elimination of the latter only ameliorates or reduces the incidence whereas elimination of the former eradicates the disease. Swamps are not a cause of malaria. Draining swamps may reduce the incidence of malaria but it is eradication of the malarial parasites that eliminates the disease. Reduction in incidence rather than elimination of the disease precludes a causal relationship.”
So, if LDL-cholesterol were the causative factor in the development of coronary artery disease, then reducing it to sub-physiological levels would seem to be the answer to eliminating heart disease. But, according to Viktor Subbotin (from whose 2012 paper I took the above two quotes) reducing LDL-cholesterol does not prevent cardiac events in 60%-70% of individuals supposedly at risk by having elevated LDL-cholesterol.
According to Subbotin:
“Unfortunately, it appears that the scientific and medical communities are focusing on and emphasizing biomarkers that can predict risk, without proof that these biomarkers cause the risk.”
Why would this be? Could it be because there exists a multibillion dollar per year industry that provides medications to reduce these biomarkers?
I somewhat get these posts as a lay person/health teacher, though they are a bit over my head...I'm trying. How can I express/teach them to my middle school students? Make it relevant to them? Any help would be appreciated.
Mike: I have a PhD in exercise physiology with a focus on vascular health, and did postdoctoral training in cellular and molecular mechanisms of vascular disease. I give that context to make the point that I 100% agree with you that these posts are SUPER heavy! I shared above that I think it's great that HQ is presenting this sort of content but it is really 'Health Science Rx' and I totally understand that there are some barriers to understanding for the 'lay-but-educated public'. I spent literally years immersed in this topic and it is presented at a level that is appropriate for someone with my experience. My doctoral students would likely struggle to grasp this information on first pass.
For your middle school students, here's what I might do. Teach them about the heart. It has 4 chambers, blood flows in this one from the lungs and out that one to the body, then on the other side receives the used stuff from the body and sends it to the lungs to exchange the used stuff for the fresh stuff. Explain that the heart is a pump. Have them count the number of times it pumps blood per minute, using the 'feel your pulse' method or maybe an app if you think they'd appreciate getting a little fancy.
Then, once they understand those basics, make them do as many burpees as possible in two minutes. Do the activity with them and see if you're fitter than a middle schooler. When everyone is done and huffing and puffing and laughing and having a great time, have them measure their heart rate again.
You'd be 100% percent scientifically justified in explaining: "Hey guys, you see how your heart rate accelerate from about 60 or 70 bpm to XX (probably 150-180 or so?) bpm after the burpees? That means we did something really good for our hearts. The harder and faster we can make our hearts beat during exercise like that, the healthier our heart and blood vessels will be".
Something like that. I do this with my college students (exercise science majors). They love it. They tell their families about it and share the experience on their social media accounts. Your middle schoolers would do the same (eventually, when they're old enough for Instagram, of course).
Thank you very much Nathan. That almost exactly what I do, in regards to resting HR and burpees or exercise. It's good to get information that I am on the right path at least.:)
Thanks again and I'll use your info for sure.
Very exciting that these posts are taking a deep dive into some vascular pathophysiology!
There is also very good evidence that atherosclerosis preferentially develops at sites of geometric irregularity in the arterial tree - branch points, bifurcations, and curvatures. The prevailing thinking is (or at least used to be?) that the site-specific development of atherosclerosis results in part from the influence of low and/or disturbed blood flow in these arterial regions. I believe these same atheroprone sites, e.g. the carotid artery, are also characterized by the presence of a developed (and likely, dysfucntional) VV.
The post seems to suggest that the VV is the initiating insult, but is it possible that the VV is itself secondary to pathologic hemodynamic stimuli, in combination with circulating pro-oxidative and pro-inflammatory factors resulting from poor dietary habits (e.g., excess refined carbohydrate consumption)?
Also related to the hemodynamic signals for vascular adaptation: one advantage of high intensity exercise is the dramatic increase in blood flow and laminar (beneficial) shear stress, even in the geometrically irregular arterial regions that are subject to low and oscillatory flow at rest. The brief interruption of resting pro-atherogenic hemodynamics seems to be one of the benefits of daily exercise for vascular health. The oddly shaped pipes of the ascending aorta, carotid bifurcation, and iliac, femoral, and popliteal branch points of the lower limb arterial tree are no match for the dramatic increases in cardiac output and metabolic demand evoked by, for example, Open 19.5. I haven’t made the measurements, but I have a strong feeling that blood flow and shear stress patterns are vigorous and uniformly antegrade under these conditions! The consequence, in theory, would be a beneficial physiological stimulus for favorable adaptations in the vascular beds exposed to the anti-atherogenic flow patterns associated with exercise.
I ask out whether hemodynamics, rather than the VV, could be the root cause of atherosclerosis out of genuine scientific interest as someone who has done *some* work in this area, but I've also been away from it for a while and don't know the latest evidence. It is no longer my main area of scientific expertise, so I’ll respectfully defer to the author of this excellent post on the matter.
I think it is great that we're having this sort of discussion in this forum!
I had a 63 yo patient today who described a family history of heart disease and assured me that she was eating a low fat diet. I said, rewind, I am going to turn everything you thought to be true on its head. And you know what, she not only heard me, but she listened. This series of bite sized explanations is perfect for her, for me, too.
The Vasa Vasorum
10