The Diabetes Remission Clinical Trial (DiRECT) demonstrated a four-month, calorie-restricted weight loss diet could reverse diabetes in a significant number of subjects (1). This 2018 analysis compared subjects in whom diabetes was successfully reversed (n = 40, “responders”) to otherwise similar subjects who remained diabetic after successful weight loss (n = 18, “non-responders”).
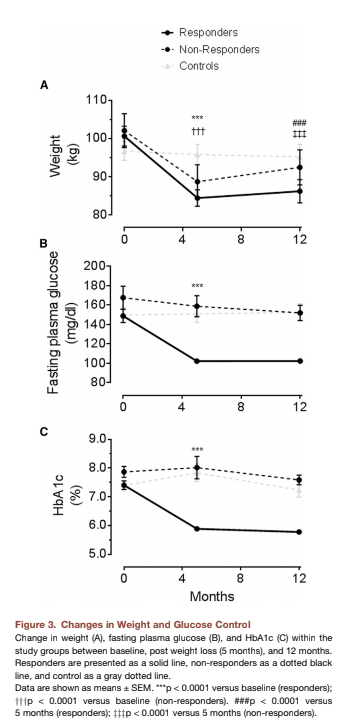
Weight loss was similar in responders and non-responders (13 to 16 kg). Alongside weight loss, liver fat content decreased dramatically in all subjects, from 16% (liver fat fraction) at baseline to 3% after weight loss, a value similar to healthy controls. Pancreatic fat content similarly decreased from an elevated baseline to healthy levels in all subjects. Previous work by these authors, as well as work featured on CrossFit.com, has linked decreased pancreatic and liver fat to improvements in glycemic control and insulin response (2).
Alongside these changes, fasting blood glucose decreased to 102 mg/dL in responders but did not change significantly in non-responders. HbA1c, accordingly, was reduced to healthy levels in responders (5.9%) but did not change significantly in non-responders. Crucially, fasting insulin decreased in all subjects, but the first-phase insulin response — that is, the amount of insulin secreted by the pancreas immediately after an elevation in blood glucose — increased to healthy levels in responders but did not change in non-responders.
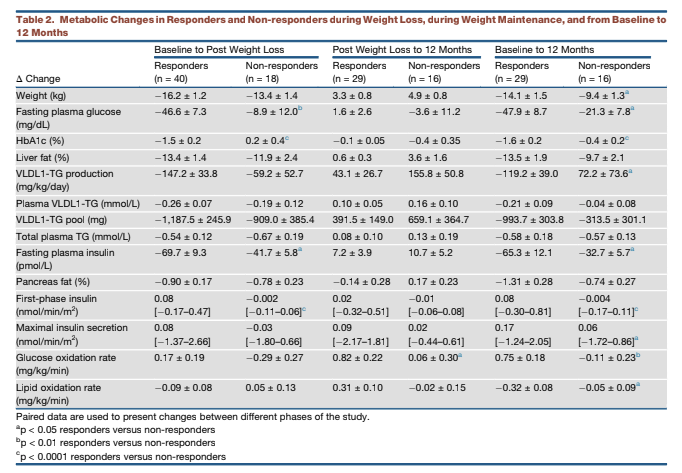
Responders and non-responders had similar average age, BMI, and fasting glucose at baseline. Non-responders had lower fasting insulin, higher plasma alanine aminotransferase (ALT), and longer average duration of diabetes than responders.
Taken together, this data indicates significant weight loss leads to liver and pancreatic fat clearance in all subjects. The pancreatic beta cells of some subjects, however, fail to return to normal levels of function even after the pancreas is cleared of fat. In these subjects, the insulin response to a glucose load (i.e., a meal) remains suppressed, so blood glucose levels and HbA1c levels remain elevated and diabetes persists even with weight loss.
Previous research has hypothesized pancreatic beta-cell stress results from high blood glucose, blood lipid, and/or insulin production levels (3). It is widely known that pancreatic beta cell function degrades over time as diabetes persists, whether as a consequence of these stressors or due to other factors.
This study contributes to the research developed in previous trials showing diabetes is reversible in the majority of subjects through the use of a calorie-restricted diet (4). Some (Lim 2011, Steve 2016) have shown a very low-calorie diet can induce diabetes reversal in as little as a few weeks. The DiRECT study builds on these smaller trials, further establishing that diabetes can be reversed through diet alone. Just as importantly, this study reinforces the importance of early intervention, as a diet started soon after diagnosis, before stressors have begun to degrade pancreatic beta-cell function, is more likely to successfully reverse diabetes.
Notes
- Primary care-led weight management for remission of type 2 diabetes (DiRECT): An open-label, cluster-randomized trial
- Pathogenesis of type 2 diabetes: Tracing the reverse route from cure to cause; Pathogenesis of type 2 diabetes: Etiology and reversibility
- The molecular mechanisms of pancreatic beta-cell glucotoxicity: recent findings and future research directions; Glucolipotoxicity of the pancreatic beta cell; Beta-cell differentiation in diabetes is important, but what is it?
- Reversal of type 2 diabetes: Normalization of beta cell function in association with decreased pancreas and liver triacylglycerol; Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance and hyperglycemia by moderate weight reduction in patients with type 2 diabetes; Very low calorie diet and 6 months of weight stability in type 2 diabetes: Pathophysiological changes in responders and nonresponders; Weight loss decreases excess pancreatic triacylglycerol specifically in type 2 diabetes