What impact can saturated fat(s) have on “cholesterol” levels?
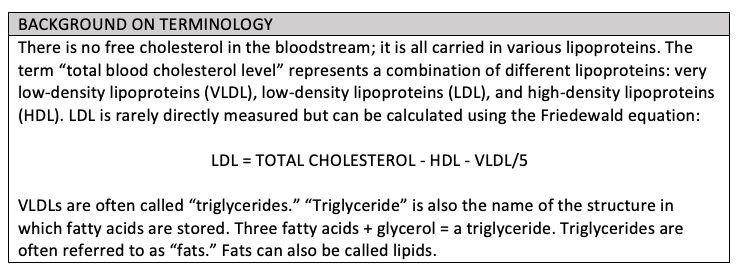
The basis of the diet-heart hypothesis is essentially that saturated fats — the type of fat normally found in animal products — are specifically capable of raising the low-density lipoprotein level (LDL), often referred to as “bad” cholesterol, thus increasing the risk of cardiovascular disease.
Ancel Keys developed the original equation to define this effect, in this case focused on total cholesterol:
Change in serum cholesterol concentration (mmol/l) = 0.031(2Dsf − Dpuf) + 1.5√Dch
In the equation, Dsf is the change in percentage of dietary energy from saturated fats, Dpuf is the change in percentage of dietary energy from polyunsaturated fats, and Dch is the change in intake of dietary cholesterol (figures used in SI unit of mmol/L).
It has now been accepted that dietary cholesterol has little or no impact on blood cholesterol levels. In the U.S. in 2015, the Dietary Guidelines Advisory Committee recognized this and stated, “Cholesterol is not considered a nutrient of concern for overconsumption” (1). This change in the guidelines was supported by several influential researchers. Patrick J. Skerrett, former Executive Editor of Harvard Health Publishing, reports:
Nutrition experts like Dr. Walter C. Willett, chair of the Department of Nutrition at Harvard School of Public Health, called the plan a reasonable move. Dr. Steven Nissen, chair of cardiovascular medicine at the Cleveland Clinic, told USA Today “It’s the right decision. We got the dietary guidelines wrong.” (2)
Although it is now recognized that dietary cholesterol does not negatively impact blood “cholesterol” level, it is still widely believed that saturated fat raises LDL-cholesterol and polyunsaturated fats lower it. No mechanism of action was proposed for either effect when the diet-heart hypothesis was first developed. The belief was primarily based on several observations.
However, the findings on saturated fat and its effect on different lipoproteins are inconsistent and depend a great deal on which dietary substances are removed or added as replacements, as an article in Medscape titled “‘Saturated Fat and Coronary Artery Disease (CAD): It’s Complicated’ illustrates:
In a meta-analysis of over 60 trials, higher intakes of saturated fat were associated with increases in both LDL-C and high-density lipoprotein cholesterol (HDL-C) and decreases in triglyceride levels [VLDL], for a net neutral effect on the ratio of total cholesterol to HDL cholesterol. [HDL cholesterol is often called “good” cholesterol].
Although saturated fats increase LDL-C, they reduce the LDL particle number. Total LDL particle number quantifies the concentration of LDL particles in various lipid subfractions and is considered a stronger indicator of CV risk than traditional lipoprotein measures.
As for stearic acid, the allegedly non-cholesterol-raising fat, while it appears to lower LDL-C relative to other SFAs, one analysis concluded that it raised LDL-C, lowered HDL-C, and increased the ratio of total to HDL cholesterol in comparison with unsaturated fatty acids. And this is one of the confounders of much nutrition research — observations about a given nutrient are highly dependent on what you compare it to. (3)
Returning to the central question: What is the mechanism by which saturated fats can raise LDL? To answer this question, we need to examine what happens to saturated fat after ingestion.
The first step is that fatty acids bind to bile salts in the bowel. Bile salts are a form of mildly adapted cholesterol, and they are synthesized in the liver and released from the gallbladder after meals. Without bile, fat cannot be readily absorbed and will pass through the GI system.
The absorbed saturated fats (fatty acids) are then packed into a very large lipoprotein (known as a chylomicron). Once a chylomicron is formed, it travels up the thoracic duct where it is then released directly into the bloodstream. Importantly, this means that chylomicrons, and thus ingested fats, do not pass through the liver.
Once chylomicrons reach the bloodstream and travel through various organs and tissues, they are stripped of their triglycerides, shrinking in size until they become a chylomicron remnant, approximately the size of an LDL molecule. These remnants are absorbed back into the liver using LDL receptors and are then broken down into their constituent parts.
Through the absorption of chylomicron remnants by the liver, a small proportion of the saturated fat that is consumed will be absorbed by the liver. However, the great majority will be directly absorbed by other tissues in the body.
This is the metabolic pathway for all types of fat: saturated, polyunsaturated, or monounsaturated. Saturated fats have no unique pathway in the way they are digested, packaged into chylomicrons, and transported around the body.
This pathway of fat metabolism has no direct connection to low-density lipoproteins (LDLs). LDL molecules are instead formed when very low-density lipoproteins (VLDLs) lose triglycerides and reduce in size. The fat/triglyceride pathway is parallel: VLDLs are created in the liver, enter the bloodstream, and gradually lose triglycerides through the action of lipoprotein lipase as they move through various organs and tissues.
The loss of triglycerides results in a reduction in size, and as they become smaller, VLDLs transform into intermediate-density lipoproteins (IDLs) before becoming low-density lipoproteins (LDLs) — at which point, most LDL molecules are removed from circulation by LDL receptors in the liver. A number of LDLs will continue to circulate and can be removed from circulation by LDL receptors, which are found on most cells in the body.
Through this process, we can see that an LDL is the remnant of a VLDL. VLDLs, in turn, can be considered to be primarily a vehicle for the transportation of triglycerides and cholesterol — which have been synthesized in the liver — to other tissues and organs.
The number of VLDLs created is primarily dependent on the rate of synthesis of fatty acids in the liver (de novo lipogenesis). Fatty acids are created when the limits of glycogen storage have been reached and glucose/fructose must therefore be converted into fatty acids as the alternative energy storage pathway. In essence, excess sugar(s) are converted to fats.
This means that a higher consumption of carbohydrates will lead to increased fatty acid synthesis in the liver, and a higher fat consumption will decrease fatty acid synthesis.
As Elizabeth Parks explains:
De novo lipogenesis is the biological process by which the precursors of acetyl-CoA are synthesized into fatty acids [fats]. In human subjects consuming diets higher in fat (>30 % energy), lipogenesis is down regulated and extremely low; typically <10 % of the fatty acids secreted by the liver. This percentage will increase when dietary fat is reduced and replaced by carbohydrate. (4)
Therefore, it is likely that a high carbohydrate diet will, in most cases, lead to a significant rise in VLDL, as demonstrated in many studies.
Parks writes:
When individuals reduce their intake of dietary fat, they frequently increase their intake of carbohydrate, and a common observation is that their blood concentration of triglycerides (TG) rises. This phenomenon, known as carbohydrate-induced hypertriglyceridemia (HPTG), has been observed in research subjects consuming high carbohydrate, low fat diets for as few as five days. (5)
In summary, what we know is that dietary saturated fat intake can have no direct impact on LDL levels. It is the level of chylomicrons that will rise if fat is ingested. The only source of LDL is VLDL, and research demonstrates that increased saturated fat will reduce de novo lipogenesis in the liver and thus decrease the synthesis of VLDLs, thereby reducing the available source of LDL. It is carbohydrate intake that increases VLDL synthesis.
The lack of any association between saturated fat and LDL levels was strongly supported by a recent study on saturated fat, reported in the U.K. press in 2018:
For the experiment, the team recruited nearly 100 volunteers, all aged over 50. They were split into three groups and every day for four weeks each ate 50g of coconut oil (about two tablespoons), or 50g olive oil — an unsaturated fat already known to lower bad LDL cholesterol — or 50g butter.
This amount of coconut oil contains more than 40g of saturated fat, twice the maximum recommended daily amount for women, according to Public Health England, but is the level previous research has revealed is necessary to show measurable changes in blood cholesterol over a four-week period.
Before the experiment, all the volunteers had their bad LDL and good HDL cholesterol measured, as well as their height, waist, blood pressure, weight and body fat percentage. Four weeks later, these tests were repeated.
The group who ate butter saw their bad LDL levels rise by about 10 per cent, as expected. But the olive oil and coconut oil saw no rise in bad LDL — despite coconut oil having more saturated fat than butter.
Even more surprisingly, while butter and olive oil both raised good HDL cholesterol by 5 per cent, coconut oil raised it by a staggering 15 percent, meaning that it seemed to have a more positive effect on cholesterol-related health than olive oil. (6)
In this study, the highest consumption of saturated fat had no effect on LDL but did raise HDL (often referred to as “good” cholesterol) by 15 percent. This study was published in the BMJ (7).
While there is no doubt that altering one’s consumption of fats and carbohydrates can alter the lipoprotein profile, there is no strong evidence that saturated fats have any impact. In some cases, the impact appears positive in that “good” cholesterol (HDL) can be raised considerably. This fits with the lack of any metabolic pathway linking saturated fats to LDL.
 Malcolm Kendrick is a family practitioner working near Manchester in England. He has a special interest in cardiovascular disease, what causes it, and what may prevent it. He has written three books: The Great Cholesterol Con, Doctoring Data, and A Statin Nation. He has authored several papers in this area and lectures on the subject around the world. He also has a blog,
Malcolm Kendrick is a family practitioner working near Manchester in England. He has a special interest in cardiovascular disease, what causes it, and what may prevent it. He has written three books: The Great Cholesterol Con, Doctoring Data, and A Statin Nation. He has authored several papers in this area and lectures on the subject around the world. He also has a blog,