This 2018 paper substantiates previous evidence indicating metformin diminishes the beneficial effects of exercise on insulin sensitivity.
Metformin is the most widely prescribed medication for the treatment of Type 2 diabetes and more recently has been promoted as a general anti-aging drug. Previous research, however, has suggested metformin may counteract the benefits of exercise, specifically the impacts of exercise on skeletal-muscular mitochondrial function and cardiorespiratory function (1).
This trial randomized patients to placebo (26 subjects) or metformin (27 subjects) alongside a 12-week aerobic exercise program. All subjects had at least one risk factor for Type 2 diabetes but were metformin naive. The exercise prescription was three weekly 45-min. sessions (treadmill, cycling, or elliptical) at 65-85% HRmax. Exercise intensity increased over the course of the trial.
Whole-body insulin sensitivity, as measured by the Matsuda Index (2), improved significantly in placebo subjects but not in subjects receiving metformin. Similarly, VO2max increased significantly in placebo subjects but not in subjects on metformin. Mean blood glucose levels before and immediately after exercise were higher in metformin-treated subjects than the placebo group.
Note: These tests were all taken 36 hours after the last metformin dose and thus represent the consequences of metformin’s effects, not the acute impacts of metformin itself. These results are summarized in Figure 1 below. Metformin did not diminish improvements in HbA1c or any fasting metabolic measures.
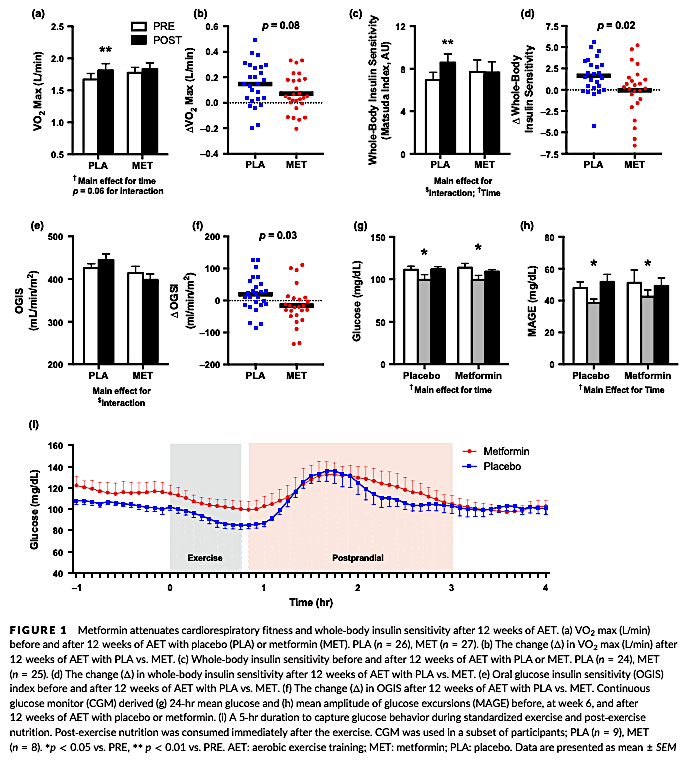
The authors observe (as Figure 1d above shows) the insulin-sensitivity response for subjects taking metformin was highly variable, with some subjects showing improvements and some showing significant decreases in whole-body insulin sensitivity. Similarly, the lack of a mean change in VO2max was due to some subjects showing a decrease in VO2max and some showing an increase.
Investigating possible mechanisms, the authors found that metformin nullified the exercise-induced increase in skeletal-muscular mitochondrial respiration seen in placebo subjects. This was not due to an increase in mitochondrial protein synthesis (i.e., it was not because metformin led muscles to produce fewer mitochondria), which suggests metformin disrupts the natural exercise-induced increase in mitochondrial respiration.
In sum, this paper points to both a specific and a broad conclusion. First, taking metformin alongside exercise inhibits two of the major benefits attributed to exercise (improvements in insulin sensitivity and cardiovascular fitness); this suggests metformin has an inhibitory rather than supplementary effect, despite improving insulin sensitivity when given without exercise. Second, the trial suggests recommendations to prescribe metformin broadly as an anti-aging medication are premature, as metformin may have impacts that accelerate key elements of age-related metabolic degeneration.
- Independent and Combined Effects of Exercise Training and Metformin on Insulin Sensitivity in Individuals With Prediabetes; Combining Short-Term Metformin Treatment and One Bout of Exercise Does Not Increase Insulin Action in Insulin-Resistant Individuals
- Matsuda Index: Study on Index for Insulin Sensitivity