What Professor Paul Sonksen calls the “‘black age’ of endocrinology” set in after researchers in the late 1950s published work revealing insulin stimulated the uptake of glucose by muscle cells. These experiments, done in vitro on isolated bits of rat muscle, were erroneously extrapolated to describe the pathophysiology of diabetes in living humans. At the time, the assumption was that hyperglycemia was driven by a lack of glucose disposal. In other words, sugar levels in the blood rose, because there was no (or insufficient) insulin to drive glucose into the cells. From this incorrect assumption, the idea arose that glucose was dependent upon insulin to get into the cells, and that exogenous insulin reduces hyperglycemia by driving glucose into the cells, particularly the muscle cells.
Although work in the 1970s disproved this theory, it has persisted. In fact, it has been taught that way for so long, it has become dogma. As Sonksen points out, “Even in well respected texts it is still common to find statements such as ‘The basic action of insulin is to facilitate glucose entry into cells, primarily skeletal muscle and hepatocytes’” (1). In discussions with multiple physicians, all remember similar instruction in medical school and continue to operate under that same false assumption.
There are plenty of glucose transporters in the cell membrane in the fasting state to facilitate glucose transport into the cells in the face of an absolute insulin deficiency as long as there exists a sufficiently high glucose gradient. There are more transporters in the cytoplasm that insulin can (and does) mobilize and bring to the cell membrane, but glucose uptake is never totally insulin dependent in humans — even in states of severe ketoacidosis.
These facts would seem to fly in the face of the reality that insulin injections do indeed quickly bring down elevated blood glucose levels in diabetic patients. But the mechanism is not that it increases glucose uptake by the cells — that is already underway. The injected insulin inhibits the liver’s output of glucose via gluconeogenesis. In diabetic patients, the liver produces and releases glucose at a much higher rate than the cells can absorb it, running blood levels ever higher. Exogenous insulin shuts off the faucet; it does not open the drain. The drain is already open. In fact, as Paul Sonksen and J. Sonksen show, exogenous insulin can actually reduce the uptake of glucose under hyperglycemic conditions (1).
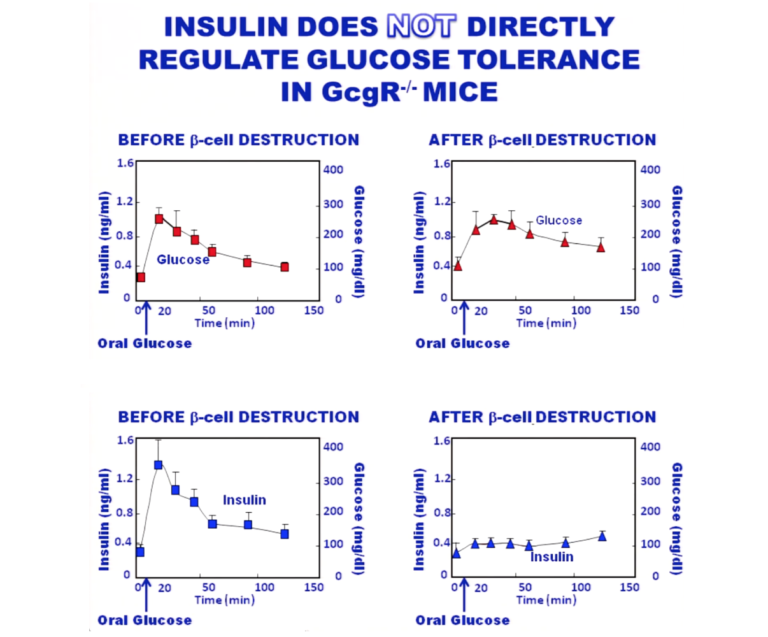
Work by Y. Lee et al. shows that in glucagon receptor knockout mice, glucose tolerance curves are essentially the same in mice with and without functional beta cells — i.e., with and without endogenous insulin (2). These animals have no functional glucagon receptors, so there is no influence of glucagon on the curves. The top graphic in the figure below shows the glucose tolerance curve in both the presence and absence of insulin. The bottom shows that insulin has been successfully eradicated in the animals, so there is no insulin effect present.
Sonksen and Sonksen detail the work done to elucidate the actions described above. They also describe the multiple actions of insulin in its inhibition of lipolysis along with its actions on glucose production and storage. This classic paper serves as an excellent primer on all aspects of glucose action, ketosis, lipolysis, and the many ways diabetes can manifest. It is well worth the time taken to study.

Drs. Michael and Mary Dan Eades are the authors of 14 books in the fields of health, nutrition, and exercise, including the bestseller Protein Power.
Dr. Michael Eades was born in Springfield, Missouri, and educated in Missouri, Michigan, and California. He received his undergraduate degree in engineering from California State Polytechnic University and his medical degree from the University of Arkansas. After completing his medical and post-graduate training, he and his wife, Mary Dan, founded Medi-Stat Medical Clinics, a chain of ambulatory out-patient family care clinics in central Arkansas. Since 1986, Dr. Michael Eades has been in the full-time practice of bariatric, nutritional, and metabolic medicine. He and his wife have been in private practice devoting their clinical time exclusively to bariatric and nutritional medicine, gaining first-hand experience treating over 6,000 people suffering from high blood pressure, diabetes, elevated cholesterol and triglycerides, and obesity with their nutritional regimen.
Together, the Eades give numerous lectures to the general public and various lay organizations on their methods of treatment. They have both been guest nutritional experts on over 150 radio and television shows, including national segments for FOX and CBS.
References
- Sonksen P, Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth. 85.1(2000): 69-79.
- Lee Y, Wang MY, Du XQ, Charron MJ, Unger RH. Glucagon receptor knockout prevents insulin-deficient type 1 diabetes in mice. Diabetes 60.2(2011): 391-7.
Comments on Insulin Is not Required for Glucose Uptake Into Cells
I truly enjoyed reading this. However, there’s definitely more to the story with blood glucose and insulin when managing diabetes. It’s sometimes way more than just this, with diabetics. Sometimes, people don’t respond to injected insulin. So essentially if they have an underlying kidney or liver disease, we can give all the insulin in the world and it never shuts off this faucet as this article states. Their organs do not respond at all. I’ve seen it, many times as a nurse. Also, if a patient is acidotic (in keto acidosis or DKA) and the anion gap is too high as a result of electrolyte imbalances, they need fluids, and an insulin drip to correct all of these problems. Glucose uptake is also dependent on electrolytes and insulin drives potassium into the cells as well. I understand the place of where this article comes from. But True Type 1 diabetics usually have way more considerations when it comes to glucose control. It’s not black and white. It’s all dependent on individual physiology. Exercise also lowers blood sugar, without insulin. And why? Because our bodies use glucose to produce ATP. ATP is used for energy and muscle contraction. Unless if someone has a faulty mechanism in doing this and that’s WAY over my head! Type II diabetics are a whole different story. They usually don’t have problems with glucose management to this extreme - YET. And they can reverse it with lifestyle changes.. I love this Biochemistry talk!
This turns what little I thought I knew about insulin on it’s head! I’m shocked, although at this point completely unamazed that everything I’ve learned has been backwards. I always thought it was weird though that Insulin activated the GLUT4 receptor, what about GLUT1, 2, and 3? I never asked and maybe I should have. Thanks for posting this, it brings a whole new light to discussions on insulin and nutrition!
Jesse,
I don't think this turns it upside down, but rather clarifies how insulin brings down blood sugar in Diabetics.
GLUT4 is still stimulated by insulin, meaning that additional GLUT4 transporters can be recruited to the cell membrane, in addition to the ones that are already there, which will accelerate glucose uptake into the cell. Unger makes the point that insulin is not "required" for glucose uptake but rather accelerates it. Yes, I was previously thinking that it "activated" the GLUT4 transporter. After reading Unger's article, I now think of it as "stimulating more" GLUT4.
My interpretation (as a non-scientist reading these articles) is that there are existing GLUT4 transporters already on the cell wall to allow glucose uptake to occur even when insulin is not present. If insulin is available, additional GLUT4 transporters are recruited, therefore glucose uptake into the cell can accelerate.
"... even in the fasting state or in a state of absolute insulin deficiency, there are sufficient glucose transporters already in place in the cell membrane to allow glucose uptake to exceed that of a normal individual when the gradient of glucose concentration across the cell membrane is sufficiently high."
From this, I interpret that the concentration of glucose outside the cell wall is what drives the uptake, rather than the concentration of insulin. The real light bulb for me was that insulin indirectly reduces the production of glucose, by inhibiting glucagon. The "turning off the faucet" analogy is great!
I had previously conceptualized GLUT4 not attached to the cell membrane unless it was stimulated by insulin, which would mean that glucose uptake couldn't occur without insulin. I didn't know that some GLUT4 were already attached to the membrane in the absence of insulin. Conceptually this all makes sense now because I knew that exercise accelerated glucose uptake by also stimulating GLUT4. So normally functioning insulin and exercise means the "drain" is working well and clearing glucose through uptake into muscles, plus glucagon is inhibited regulating glucose production (the faucet).
My understanding is that GLUT1, GLUT2, GLUT3 and GLUT5 are not insulin dependent, but are also not found in the skeletal muscles.
Still seems consistent with Insulin being the "Master hormone". I feel like my brain has been stretched!
Would’ve loved to see a discussion the the further work done by Unger. A quick search reveals he has furthered this line of inquiry quite significantly.
Great description. You had pointed out to me, a while ago, that Sonksens never received adequate credit for the work. This still seems to be true although the work has been reproduced in whole humans still not giving them credit. On Unger's work (your reference (2), it was made out that this was some kind of radical overthrowing of the primacy of insulin and that glucagon controlled things. This is not an accurate interpretation. While Unger's work is beautiful, insulin is still more or less the master hormone. It is that it works by keeping glucagon under control., that is, they work together: insulin essentially telling glucose when to break down glycogen and put glucose into the blood (and when to allow gluconogenesis to keep up). I have a YouTube describing this and the general working of this system: https://www.youtube.com/watch?v=STzB2USmKBg. .
Insulin Is not Required for Glucose Uptake Into Cells
5