Science often lurches along by serendipity. Take for instance the accidental discovery of saccharin at Johns Hopkins University in 1879, when Constantin Fahlberg, a research chemist, neglected to wash his hands before lunch and was surprised to discover a chemical he’d spilled on his fingers made the bread he was eating taste sweeter. He published his findings the next year in co-authorship with the head of the lab, but even back then, it appears those in the halls of academic research were subject to perfidy in the face of lucre’s siren call. In short order, Fahlberg patented the substance he’d isolated (without including his co-author) and began mass-producing it (also without his co-author) for sale to a sweet-loving populus. In the right place at the right time, saccharin’s rise in popularity benefitted from sugar rationing during WWI, but it didn’t really hit its stride until almost half a century later with its introduction into diet soft drinks.
The story might have ended there, but Fahlberg’s sloppy, finger-licking lab technique (and academic back-stabbing) launched a quest, still ongoing in food manufacturing: develop a suitable replacement for sugar that won’t rot your teeth, make you fat, make your face break out, or otherwise ruin your health. Finding a substitute that would allow people, especially diabetics and others intolerant of sugar, to continue to enjoy sweet treats without metabolic consequence would be akin to discovering the ark holding the holy grail, not to mention hitting the jackpot. Thus, the entrants into the sugar replacement race, since those early saccharin days, have been many and varied. Some, such as cyclamates and aspartame, are artificial lab creations like saccharin; some, such as stevia and monk fruit extract, are derived from nature; and some, such as sucralose and the plethora of sugar alcohols, are nature-lab hybrids, from erythritol to xylitol.
Non-sugar artificial sweeteners (NAS) have been alternately hailed and demonized throughout their history; hailed as the sweet, low-calorie saviors of the diabetic and obese on the one hand and vilified on the other as destroyers of health. Wariness over NAS dates from the nearly half-century-old research suggesting cyclamates cause bladder cancer (1), research based on a mouse study that employed supernormal doses of the stuff, equivalent to a human’s consuming over 550 cans of diet soda a day. The study resulted in a ban of the sweeteners in the U.S. (though not European) market. Additional concerns emerged out of the well-documented gastrointestinal (laxative and bloating) side effects occasioned from robust consumption of some sugar alcohols (2), and from the purported hyperactivation of excitatory neurochemical pathways by aspartame (3). But a recent bit of research raises an even more troublesome specter, suggesting some of these non-sugar sweeteners may contribute to the development of Type 2 diabetes (T2DM) and cardiovascular disease.
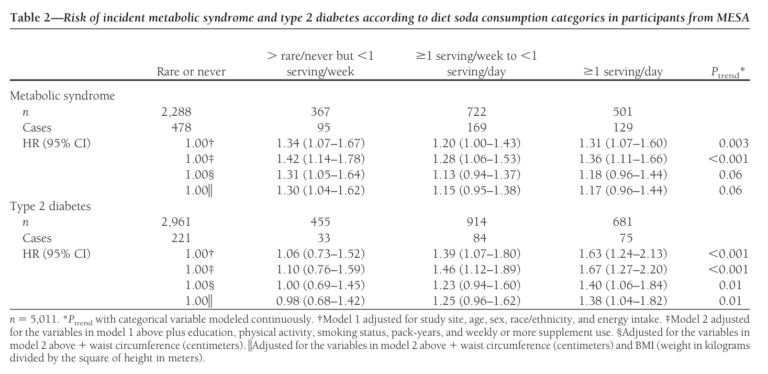
A 2009 observational study by Nettleton et al. looked into the association between artificially sweetened beverage intake and diabetes and claimed to find a striking uptick in diabetes risk from diet soda consumption (4). In fact, the study found a 67% relative risk increase was associated with the daily consumption of one or more servings of diet soda. Closer examination of the data showed an increase of 3.6/100 people (a 48% absolute increase) when comparing the extremes of consumption — i.e., comparing those never consuming diet sodas to those consuming at least one or more a day.
But what, if anything, does this really mean? Are those who never drink a soda of any sort the same as those who consume one every day or even at every meal? Would they likely eat the same sorts of foods? Would one group be more likely to consume fast food than the other? Would one group be more likely to focus on food quality? Would people perhaps already predisposed to being overweight be more likely to try drinking non-sugar-sweetened (aka diet) beverages in an effort to curb calories? Would these people drink such beverages in conjunction with a whole-food, healthful diet, or would they consume the beverages as the nod to calorie reduction in an otherwise poor-quality meal, filled with all manner of refined starch and/or sugar (bread, pasta, potatoes, corn, rice, desserts)? We don’t know from the data.
A large meta-analysis published in 2014 by Greenwood et al. further looked into the association and concluded there was a clear dose-response trend for the development of diabetes with sugar-sweetened beverages and a similar but more tenuous trend for that effect with artificially sweetened beverages. The bottom line, however, is that it’s all observational data and can be confounded in a variety of ways.
If the association were to prove valid — and it always bears repeating that correlation isn’t causation — the implications for health would be staggering in light of the high prevalence of both diabetes and diet soda consumption. In 2017, the CDC estimated there to be 100 million diabetics and pre-diabetics in the U.S. alone, with double that or more worldwide. Coupled with a 2016 study by Park et al. (6) that used 2013 data to estimate 30% of adults in the U.S. drink at least one diet soda a day (a frightening increase over the 20% estimate in 2010), a perfect storm scenario takes shape. And we should bear in mind that a great many people (adults and, sadly, kids) clearly drink far more than a single 12-ounce diet soda per day, courtesy of the bottomless refills to be had at myriad fast food establishments on every street corner and dotting the landscape from coast to coast.
While it’s fine to note the possible association between diet soda consumption and diabetes risk, it’s far more important to determine any plausible mechanisms behind it. Several reasonable hypotheses have emerged as research targets of late. One interesting one involves disruption of the gut microbiome.
Microbiome Disruption in the Development of T2DM
Research support for changes in the gut microbiome occasioned by non-sugar artificial sweeteners (NAS) comes from both mouse and human data in work by Suez et al., published in Nature in 2014 (7). The researchers demonstrated induction of glucose intolerance (e.g., essentially pre-diabetes) in both lean and obese mice fed supplemental NAS. The intolerance could be abolished by the concomitant addition of broad-spectrum antibiotics to the regimen, which suggests the living microbiome plays some role. Glucose intolerance could likewise be readily transmitted from now glucose-intolerant, NAS-drinking mice to normal, germ-free mice simply by fecal transfer, which further suggests a causative or at least contributory role for the microbiome in the development of the diabetic metabolic derangement — interesting, if you’re a mouse, but surprisingly, essentially the same thing happened when humans were studied.
Suez et al. sought to pin down a causative role for NAS and glucose intolerance in humans vis-à-vis changes in the gut microbiome. Subjects who were not previously NAS consumers were dosed three times a day for several days with a saccharin load and examined in comparison to their baseline values (8). Some readily responded and others did not. The responders, even in so short an exposure, exhibited both an erosion of glucose tolerance and changes in the makeup of their microbiome. More interesting yet, when researchers transplanted this altered human microbiome via fecal transfer to normal germ-free, glucose-tolerant mice, the mice developed glucose intolerance.
Amplification of the Glucose/Insulin Signal
Another theory receiving research attention that may implicate NAS in the genesis of T2DM hinges on a demonstrated effect (in both animals and humans) of these non-caloric sweeteners on stimulating glucose absorption and spiking insulin. Artificial non-sugar sweeteners — not on their own but in synergy with a glucose load — act to amplify the release of glucagon-like peptide-1 (9). GLP-1 is an intestinal incretin hormone released when food (primarily glucose) enters the small intestine; it serves to amplify (by up to 75%) the glucose-mediated rise of insulin levels in the blood, depresses glucagon release, and sets off a whole host of physiologic responses (10), including delayed gastric emptying and slowed intestinal transit time, all of which influence blood sugar and insulin levels. Additionally, the intense sweetness of NAS appears to stimulate gut “sweet receptors’” that further increase the uptake of glucose from gut to blood.
The interplay of these physiologic forces is complex, and their significance is as yet not clear, but this research at least reminds us that even though NAS aren’t sucrose and don’t contain calories, that doesn’t mean they don’t exert profound physiologic effects. The amplification (and potential disruption) of the glucose/insulin signaling pathways by NAS may turn out to be an important mechanism in the march from normal blood sugar and insulin to hyperinsulinemia and hyperglycemia.
We’re left with two possible mechanisms that could implicate NAS as a possible contributor to the steep rise in T2DM we’ve seen worldwide since the 1980s. NAS are clearly not the only contributors — for that we would first look to refined, concentrated sources of sugars and starches — but sugars and NAS both clearly impact our insulin-glucose signaling pathways, with NAS serving more to potentiate sugar’s effects. While poorly nutritive or even non-nutritive for us, sugar provides and NAS may provide a gluttonous feast for the members of our microbiome, favoring some, starving others, and in the end altering the microbiome’s composition. Perhaps gluttony, even among our resident bacteria, is unhealthy.
Does any of this prove causation? No, not yet, but it offers up some intriguing direct clinical laboratory support for these theories, which beg for more study. And, the associations are intriguing enough, perhaps, to give us yet another reason to avoid regularly overconsuming concentrated sweet foods, artificial or not.

Drs. Michael and Mary Dan Eades are the authors of 14 books in the fields of health, nutrition, and exercise, including the bestseller Protein Power.
Dr. Mary Dan Eades was born in Hot Springs, Arkansas, and received her undergraduate degree in biology and chemistry from the University of Arkansas, graduating magna cum laude. After completing her medical degree at the University of Arkansas, she and her husband have been in private practice devoting their clinical time exclusively to bariatric and nutritional medicine, gaining first-hand experience treating over 6,000 people suffering from high blood pressure, diabetes, elevated cholesterol and triglycerides, and obesity with their nutritional regimen.
Together, the Eades give numerous lectures to the general public and various lay organizations on their methods of treatment. They have both been guest nutritional experts on over 150 radio and television shows, including national segments for FOX and CBS.
Notes
- Taubes G. The Case Against Sugar. London, England: Portobello Books, 2017. pp. 143–144.
- Ravry MJ. Dietetic food diarrhea. JAMA 244.3(July 18, 1980): 270.
- Rycerz K, et al. Effects of aspartame metabolites on astrocytes and neurons. Folia Neuropathol. 51.1(2013): 10-17.
- Nettleton JA, et al. Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 32.4(April 2009): 688-694.
- Greenwood DC, et al. Association between sugar-sweetened and artificially sweetened soft drinks and type 2 diabetes: Systematic review and dose-response meta-analysis of prospective studies. British Journal of Nutrition 112.5(Sept. 14, 2014): 725-34.
- Park S, Xu F, Town M, Blanck HM. Prevalence of sugar-sweetened beverage intake among adults – 23 states and the District of Columbia, 2013. MMWR Morb Mortal Wkly Rep. 65.7(2016): 169–74.
- Suez J, et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 514.7521(2014): 181-186.
- Saccharine was the only NAS tested in this Suez et al. study, though similar responses have been demonstrated for acesulfame K and sucralose. Naturally sweet herbs, such as stevia or monk fruit, may or may not have this effect but weren’t studied in this case. Stevia has actually shown some degree of benefit in lowering post-prandial glucose and insulin response.
- Brown RJ et al. Ingestion of diet soda before a glucose load augments glucagon-like peptide-1 secretion. Diabetes Care. 32.12(Dec. 2009): 2184-2186.
- Nauck MA and Meier JJ. Incretin hormones: Their role in health and disease. Diabetes Obes Metab. 20.Suppl. 1(2018): 5-21.