This 2004 article reviews the mechanisms by which exercise improves insulin sensitivity. Multiple streams of evidence suggest exercise has beneficial effects and sedentary behavior detrimental effects on insulin action and blood glucose control. The authors note that skeletal muscle insulin resistance is “the hallmark feature” of the obese and/or diabetic.
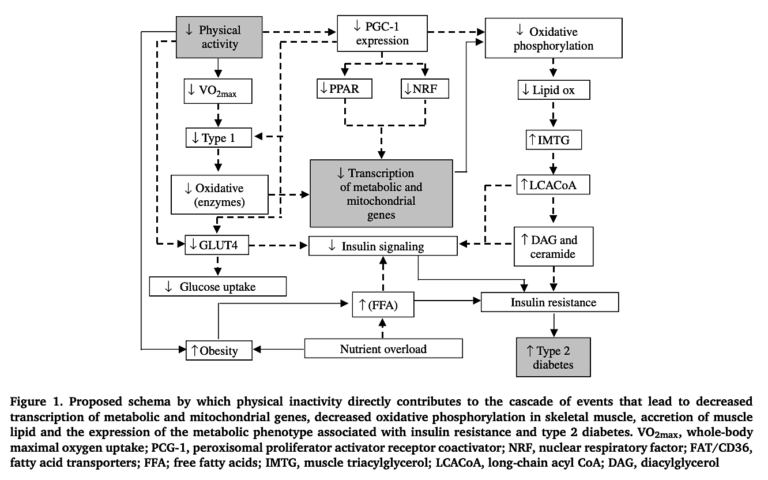
They discuss a variety of potential mechanisms by which inactivity could lead to skeletal muscle insulin resistance and activity could reverse it. Specifically:
- Total muscular mitochondrial area is reduced in Type 2 diabetics, with a consequent reduction in muscular oxidative capacity; exercise increases muscular respiratory and oxidative capacity.
- During exercise, insulin-stimulated glucose uptake is severely impaired in Type 2 diabetics compared to nondiabetics. A key mechanism by which insulin stimulates glucose uptake in muscle is through the translocation of GLUT4 transporters to the surface of the cell, where they pull glucose out of the blood. In the muscle cells of diabetics, levels of intracellular GLUT4 are normal, but insulin fails to stimulate their translocation to the outside of the cell — i.e., insulin’s signal is failing to reach the right proteins to stimulate glucose uptake. Exercise training has been shown to reverse these deficits and normalize the muscle’s ability to take in glucose when stimulated by insulin.
- Exercise training increases the muscle’s ability to oxidize fat, which is impaired (for reasons directly related to the mitochondrial deficits noted above) in diabetics.
In other words, skeletal muscle insulin resistance — and thus, to a large extent, overall insulin resistance — in diabetic subjects is due to reduced mitochondria production and/or activity and reduced insulin signaling in muscle cells. Exercise has been shown to reverse these deficits.
As the authors conclude:
Given the strong evidence for a direct role of physical activity in the prevention of insulin resistance, and the fact that exercise training increases mitochondrial biogenesis and improves glucose tolerance and insulin action in individuals with insulin resistance and type 2 diabetes, the question of why such a potent modulator of these conditions is not more commonly prescribed is perplexing and should be of utmost concern to medical health care professionals worldwide. To continue to attack the growing health burden by investing almost exclusively in strategies that target secondary and tertiary treatment of chronic disease states (i.e. pharmaceutical interventions) is extremely short sighted: primary defence mechanisms (i.e. exercise/diet and lifestyle interventions) will decrease disease prevalence by preventing these conditions in the first place!
Figure 1 below summarizes these mechanisms.
Comments on Exercise as a Therapeutic Intervention for the Prevention and Treatment of Insulin Resistance
You cannot reverse Type 2 Diabetes with exercise alone. The intervention, first and foremost, requires carbohydrate restriction using a ketogenic diet (www.virtahealth.com). The main strength of combining the ketogenic diet with a fitness program like CrossFit is the optimization of the insulin sensitivity that rises with keto adaption in the process of diabetic reversal.
Peter, I think you're absolutely right to note this; at the very least, any exercise dose/program that could reverse diabetes by itself isn't realistic. Conversely, Virta and others have shown that diet alone can reverse diabetes, even among diabetics in more advanced stages of the condition. I suspect, however, that when dietary improvements are supplemented with exercise, we may see faster and/or more significant benefits. For example, I would expect exercise could help clear fat stores in the liver and muscle tissue, and so restore insulin sensitivity in those areas, more quickly than diet alone. I don't think we necessarily have data to support that, and frankly the most effective dietary interventions (i.e., fasting and ketogenic diets) may be effective enough that they don't need to be bolstered, but the mechanisms lead me to believe exercise could play a role, particularly in harder-to-treat patients.
While the mechanisms presented here are complex, the overall biological behavior is fairly simple. Our muscles are one of the best tools our body has to manage our blood glucose levels, and so to keep our need for insulin in check. When our muscles become less responsive to insulin, and less able to pull glucose out of the blood, more insulin will be required to effectively modulate our blood glucose levels - and so the spiral toward insulin resistance begins. If, as this article argues, exercise plays a specific role to short-circuit this progression (by either preventing the muscles from developing insulin resistance in the first place or reversing it once it has developed), it may be a particularly powerful tool to prevent or reverse progression toward metabolic disease. The questions that would follow, then, are (1) what sorts of exercise are the most effective tools to prevent / reverse muscular insulin resistance (dose & form) and (2) how great an impact can exercise have, both by itself and as a supplement to dietary changes? I expect we can answer most of these questions simply through practice, and observing what does and does not put a dent in these conditions.
As Russ noted above, these questions may be critically important. Both the dose and the form of exercise must matter, as well as the broader context in which that exercise is done; if "exercise" is entirely genericized (either to the extreme of referring to all activity by a single term, or through blunt abstraction simply to "minutes of movement" or something similar), we'll lump ineffective treatments in with effective ones. Per Russ's closing comments, we already know what might happen in this case, as individuals and organizations without patients' best interests at heart co-op a valuable treatment, and the perceived public health impact of the intervention drops. The best tool to protect against this may be better understanding of where the border between effective and ineffective intervention lie (even if that border is fuzzy or variable), and with it tools to direct patients toward the former and away from the latter, but I don't think that's something the current research can clearly provide.
"why such a potent modulator of these conditions is not more commonly prescribed is perplexing and should be of utmost concern to medical health care professionals worldwide."
It's not that perplexing. The pharmaceutical industry has done a better job at marketing and lobbying drugs than the soda-exercise complex has done at marketing physical activity. For now.
Should, however, the current absence of activity presciption it be "of utmost concern?" The answer depends largely on what form activity prescription would take.
Would it follow the Coca-Cola / ACSM Exercise is Medicine plan? That is, would this new focus on doctor prescription of physical activity ignore nutrition and largely overlook intensity and functionality? If so, patients probably be better off without it. Or would this new paradigm recognize the fundamental importance of nutrition, and the value of actually training movements required in daily life.
More important, who would decide what form the activity would take? Would the doctors be able to recommend their own trainers, gyms and methods, based on their own experience, or would bureaucrats and highly-centralized authorities confine them, and their patients, to particular certain gyms and trainers (read: the ones associated with the most powerful lobbying forces).
And, how would doctors assess patient progress? Would clients be "incentivized" to wear unreliable devices such as Fitbits, violating their civil liberties for ineffective, if not downright iatrogenic, results (as Ezekiel Emanuel and others have suggested)? Or, would the physicians use actual fitness testing such as time taken to get off the ground, number of squat-to-stands performed in 20 seconds, etc.?
The same questions largely apply to the push to involve nutrition in medicine. The devil remains in the details.
Completely agree, Russ Greene! The prescription mainstream medicine would proffer to the DMT2 patient is a low fat diet replete with many servings of 'complex' carbohydrates. And the preferred fat would be 'heart healthy canola oil' and other 'vegetable oils'. The exercise they'd recommend would be something on the order of walking with light hand weights at most. Wrong diet. Wrong exercise recommendation. A plan guaranteed to be ineffective.
Increasing fat in the diet (particularly saturated varieties) works to increase mitochondrial density. Dropping sugar and carbohydrate intake shifts the metabolic machinery toward fat burning in those more plentiful mitochrondria. And coupling the correct nutritional structure with an exercise plan that combines regular high intensity aerobic activities of sufficient duration to boost fat use with maximum intensity resistance training to achieve anaerobic (ie, glucose burning) metabolism will work. I think I know of such a plan!
Exercise as a Therapeutic Intervention for the Prevention and Treatment of Insulin Resistance
5